Review Article
Intra-Arterial Hepatic Perfusion for Metastatic Melanoma of Cutaneous Origin
Sean J.Judge, Amanda R.Kirane and Sepideh Gholami*
Department of Surgery, University of California, USA
*Corresponding author: Sepideh Gholami, Department of Surgery, University of California, Davis Comprehensive Cancer Center, 2279 45th St., Sacramento, CA 95817, USA
Published: 22 Oct, 2018
Cite this article as: Judge SJ, Kirane AR, Gholami S. Intra-
Arterial Hepatic Perfusion for Metastatic
Melanoma of Cutaneous Origin. Clin
Surg. 2018; 3: 2165.
Abstract
Intra-arterial Hepatic Perfusion (IHP) is a chemotherapeutic strategy that has been in use for several
years. Its application in non-resectable liver metastases has gained increased acceptance following
favorable results from recent clinical studies. Most of these published studies focus on outcomes of
metastatic colorectal and ocular melanoma due to the high frequency of isolated liver metastases. To
better understand the role of IHP in metastatic melanoma, we reviewed the pertinent literature with
a focus on cutaneous melanoma. Here we present a brief report of IHP for metastatic melanoma of
cutaneous origin. We have highlighted the available data on patient outcomes with attention to the
unique morbidity and mortality, and future directions of IHP therapy.
Keywords: Intra-arterial hepatic perfusion; Regional therapies; Metastatic melanoma; Cutaneous melanoma
Introduction
Metastatic cutaneous melanoma portends a poor prognosis with median survival in the range of 6 to 10 months and 5-year survival less than 5% [1]. With the development of systemic immunotherapy utilizing checkpoint inhibition, long term survival has now become a possibility for selected patients with stage IV disease. In the era of improved systemic therapy, the role of regionally directed therapies remains in question. We report on the role of Intra-arterial Hepatic Perfusion (IHP) for non-resectable metastatic cutaneous melanoma to the liver.
Indication and Description of Procedure
Current clinical trials include patients with non-resectable metastatic melanoma limited to
the liver. Although the vast majority of melanoma incidence is related to cutaneous disease, liver
specific relapse is more commonly observed in ocular melanoma [2]. Importantly, to tolerate the
extracorporeal filtration system necessary for isolated perfusion, patients must be amenable to
systemic anticoagulation.
Intra-arterial hepatic perfusion via a percutaneous approach utilizes an extracorporeal filtration
system to maximize hepatic concentration and minimize systemic exposure. Briefly, this is completed
through isolating the hepatic circulation by 1) cannulating the hepatic artery via the femoral artery,
2) occluding the suprahepatic inferior vena cava via the internal jugular vein, and 3) occluding
the infrahepatic IVC via the femoral vein. The infusate enters the hepatic circulation through the
hepatic artery and is cleared by the hemofiltration system draining from the suprahepatic IVC. The
liver is further excluded from systemic circulation via hepatic bypass from the infrahepatic IVC
and return via the internal jugular vein cannula. CT angiography of the liver is required for preoperative
planning to ensure no inadvertent extrahepatic perfusion.
Outcomes
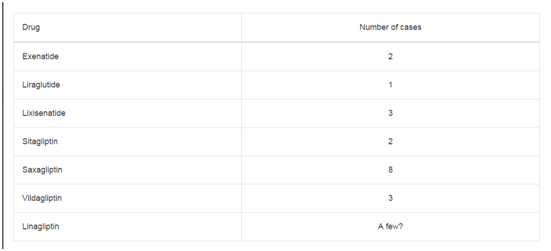
Of the larger studies reported, only four enrolled patients with metastatic melanoma of cutaneous origin [3-6], with a cumulative total of 18 patients treated with IHP. Of these studies, only one reports the individual outcomes for the cutaneous melanoma cohort [4]. All patients in this study experienced at least a partial response; however, in one patient, lung metastases developed, and in another, hepatic recurrence occurred within 13 months. In a large retrospective review of a prospectively collected database, 91 patients underwent IHP for liver metastases of colorectal and non-colorectal primary cancers over a ten year period [3]. Only three patients had a primary cutaneous melanoma in this study. Response rates for the colorectal, melanoma, and cholangio carcinoma cohorts were 68%, 57%, and 100%, respectively. Analysis of response rate for the subset of patients with primary cutaneous melanoma was not reported. Therefore, it remains unclear if the outcomes in metastatic ocular melanoma hold true for melanoma of cutaneous origin. A synopsis of these studies is presented in Table 1.
Table 1
Morbidity and Mortality
Although introduction of the percutaneous approach abrogated
the need for a laparotomy incision, significant procedural and nonprocedural
morbidity and mortality remain. The phase III trial by
Hughes et al. [5] suggests that adverse events in the peri-procedural
period, defined by the first 72 hrs after the procedure, are common,
occurring in approximately 90% of patients. The most common
adverse events in this period were thrombocytopenia and anemia. In
the post-procedural time, defined as the first 30 days after the periprocedural
period, adverse events remain similar, occurring in 91%
of patients in this trial. In the same trial, three deaths occurred in the
treatment arm and one death occurred in the crossover arm. Of the
three deaths in the treatment arm, one was attributed to neutropenia,
another to sepsis, and a third to liver failure. In the crossover arm,
mortality was attributed to a gastric perforation. Specific timing of
mortalities was not reported in the trial.
The adverse events described by Vogl et al. [4] reflect a similar
trend as observed by Hughes et al. However, two described events
were attributed to systemic heparinization and the resultant
coagulopathy with one fatal retroperitoneal hematoma at 30 hrs postinfusion.
Both studies highlight a near ubiquitous rate of adverse
events and a mortality rate between 4% (4/70) and 7% (1/14). There
is clear potential for significant improvement with the use of newer
hemofiltration systems and novel infusate regimens.
Future Directions
Melphalan has been the standard infusate for IHP in metastatic cutaneous melanoma due to its effect on dividing and resting cancer cells and the ability to achieve significantly higher maximal dosing when the liver is isolated from systemic circulation. This also holds truth for isolated limb infusion for in-transit cutaneous melanoma of the extremity. Given the parallels between the two procedures, ongoing advances in Isolated Limb Infusion (ILI) may show promise in IHP. One such advance is the addition of systemic ADH-1, a disruptor of N-cadherin adhesion complexes, to regional melphalan. Response outcomes have been mixed, but there may be a role for ADH-1 in melanoma sensitization as a component of multimodality treatment [7,8]. Lastly, the engineered oncolytic virus Talimogene Laherparepvec (T-VEC) has shown promise as intratumoral therapy. Proposed mechanism of action involves both a lytic effect on infected tumor cells and a pro-immune effect via downstream signaling [9]. Results of the OPTiM Trial comparing intralesional T-VEC vs. subcutaneous GM-CSF showed that patients treated with T-VEC had improved durable response (16.3% vs. 2.1%) and improved overall response rates (26.4% vs. 5.7%) [10]. Ongoing clinical trials of visceral injection of intralesional therapies are being conducted but remain in early phases.
Conclusion
The growing body of literature suggests that intra-arterial hepatic perfusion for malignant melanoma of cutaneous origin is a treatment modality with great potential. IHP improves hepatic and overall progression free survival and may be a viable option for stage IV disease limited to the liver. The encouraging outcomes for this unique cohort are limited, and ongoing accrual of cutaneous melanoma patients into clinical trials will strengthen this conclusion. Concerns regarding morbidity and mortality of IHP are well founded and any risk/benefit calculation should be carefully determined prior to offering or proceeding with such therapy. However, with improvements in technique and hemofiltration systems, hematologic complications should continue to improve. There is a growing arsenal of novel therapies and multimodality regimens, and such results offer hope for continued advancement.
References
- Tsao H, Atkins MB, Sober AJ. Management of cutaneous melanoma. N Engl J Med. 2004;351(10):998-1012.
- Diener-West M, Reynolds SM, Agugliaro DJ, Caldwell R, Cumming K, Earle JD, et al. Development of metastatic disease after enrollment in the COMS trials for treatment of choroidal melanoma: Collaborative Ocular Melanoma Study Group Report No. 26. Arch Ophthalmol. 2005;123(12):1639-43.
- Magge D, Choudry HA, Zeh HJ 3rd, Cunningham DE, Steel J, Holtzman MP, et al. Outcome analysis of a decade-long experience of isolated hepatic perfusion for unresectable liver metastases at a single institution. Ann Surg. 2014;259(5):953-9.
- Vogl TJ, Zangos S, Scholtz JE, Schmitt F, Paetzold S, Trojan J, et al. Chemosaturation with percutaneous hepatic perfusions of melphalan for hepatic metastases: experience from two European centers. Rofo. 2014;186(10):937-44.
- Hughes MS, Zager J, Faries M, Alexander HR, Royal RE, Wood B, et al. Results of a Randomized Controlled Multicenter Phase III Trial of Percutaneous Hepatic Perfusion Compared with Best Available Care for Patients with Melanoma Liver Metastases. Ann Surg Oncol. 2016;23(4):1309-19.
- Abbott AM, Doepker MP, Kim Y, Perez MC, Gandle C, Thomas KL, et al. Hepatic Progression-free and Overall Survival After Regional Therapy to the Liver for Metastatic Melanoma. Am J Clin Oncol. 2018;41(8):747-53.
- Beasley GM, McMahon N, Sanders G, Augustine CK, Selim MA, Peterson B, et al. A phase 1 study of systemic ADH-1 in combination with melphalan via isolated limb infusion in patients with locally advanced in-transit malignant melanoma. Cancer. 2009;115(20):4766-74.
- Beasley GM, Riboh JC, Augustine CK, Zager JS, Hochwald SN, Grobmyer SR, et al. Prospective multicenter phase II trial of systemic ADH-1 in combination with melphalan via isolated limb infusion in patients with advanced extremity melanoma. J Clin Oncol. 2011;29(9):1210-5.
- Corrigan PA, Beaulieu C, Patel RB, Lowe DK. Talimogene Laherparepvec: An Oncolytic Virus Therapy for Melanoma. Ann Pharmacother. 2017;51(8):675-81.
- Harrington KJ, Andtbacka RH, Collichio F, Downey G, Chen L, Szabo Z, et al. Efficacy and safety of talimogene laherparepvec versus granulocyte-macrophage colony-stimulating factor in patients with stage IIIB/C and IVM1a melanoma: subanalysis of the Phase III OPTiM trial. Onco Targets Ther. 2016;9:7081-93.