Research Article
Remote Intracranial Hemorrhage after Spinal Surgery: Possible Etiology and Incidence
Toshimi Aizawa1*, Hiroshi Ozawa2, Yoshihiro Ashina1, Ko Hashimoto1, Haruo Kanno1, Toshimitsu Eto1 and EijiItoi1
1Department of Orthopaedic Surgery, Tohoku University School of Medicine, Japan
2Department of Orthopaedic Surgery, Tohoku Medical and Pharmaceutical University, Japan
*Corresponding author: Toshimi Aizawa, Department of Orthopaedic Surgery, Tohoku University School of Medicine, 1-1, Seiryo-machi, Aoba-ku, Sendai, Miyagi Prefecture, Japan
Published: 02 Aug, 2018
Cite this article as: Aizawa T, Ozawa H, Ashina Y,
Hashimoto K, Kanno H, Eto T, et al.
Remote Intracranial Hemorrhage after
Spinal Surgery: Possible Etiology and
Incidence. Clin Surg. 2018; 3: 2058.
Abstract
Background: Remote Intracranial Hemorrhage (RIH) is a rare but potentially lethal complication
related to Cerebro Spinal Fluid (CSF) drainage. Spinal surgery has a chance of durotomy or dural
tear. However, the exact incidences of RIH resulting from spinal surgery remain uncertain.
Objective: The aim of the present study was to prospectively evaluate the incidence of RIH, and the
relationship between RIH and CSF drainage volume.
Methods: A total of 691 patients underwent spinal surgery in our department between May 2007
and April 2016. Among these, 175 had durotomy or dural tear, which were evaluated with brain
CT the day after surgery, regardless of brain symptoms. The clinical features of RIH and drainage
volume were assessed.
Results: Three patients were affected by RIH, including two asymptomatic. The incidence among
all spinal surgeries was 0.4% and among durotomy or dural tear was 1.7%. Patients with RIH had
significantly more drainage totally and per 24 hours after surgery than those without (589 ± 157
ml vs. 314 ± 968 ml, p=0.01; 898 ± 185 ml vs.157 ± 160 ml, p=0.003). RIH was detected in the
cerebellum alone, in both the cerebellum and cerebrum, and in the cerebrum alone in one each,
respectively. One patient with hydrocephalus was treated conservatively and completely recovered
from their brain symptoms within 17 days.
Conclusion: The incidence of RIH in this study was higher than expected. RIH was closely related
to CSF drainage volume, in particular, with large volume loss within a short time.
Keywords: Remote Intracranial Hemorrhage; Spinal surgery; Prospective study; cerebrospinal fluid; complication
Introduction
Remote Intracranial Hemorrhage (RIH) is a rare but potentially lethal complication related to
Cerebrospinal Fluid (CSF) drainage [1,2]. RIH is most likely to develop in the cerebellum, and thus
has been termed “remote cerebellar hemorrhage” in the previous reports, although it can occur in
various intracranial locations [3,4]. RIH has recently become a well-recognized complication during
and after thoracoabdominal aortic repair and brain surgery [3,4]. In the thoracoabdominal aortic
repair, lumbar CSF fluid drainage is commonly used to reduce the risk of spinal cord injury caused
by ischemia [3,5]. The reported incidence of RIH associated with thoracoabdominal aortic repair
is between 0.5% and 3.5%; that after supratentorial surgery is between 0.2% and 4.9% [2-5]. When
RIH occurs during thoracic aortic repair, a high associated mortality of 40% has been reported [3].
During spinal surgery, durotomy is performed to remove intradural lesions. Dural tears can
also occur accidentally or deliberately; for example, ossified dura mater in the ossification of the
ligamentum flavum is occasionally removed with the corresponding ossified ligamentum [6]. RIH
can occur due to CSF leakage related to spinal surgery. Severe disability or death has been described
in 26.6% of patients with RIH after spinal surgery, which strongly indicates that spine surgeons
should be well informed about this complication [7,8]. However, almost all previous reports were
case reports and the exact incidence of RIH resulting from spinal surgery and the association
between the volume of CSF leakage and the occurrence of RIH are uncertain. The purpose of the
present study was to prospectively clarify these two questions. The volume of CSF leakage during
surgery cannot be measured precisely since it is mixed with blood. Intraoperatively, the volume
of hemorrhage during surgery should be affected by the operative
time, the types of surgery, the size of exposure, and so on and that
of CSF leakage should be also affected by the timing and size of
dural rupture, the level of spinal surgery, and the closing procedures
of dural tear. In addition, the volume of CSF leakage with bleeding
during surgery should not be controlled. On the other hand, the
postoperative volume of CSF and hemorrhage might be controlled
using a suction drainage system. Therefore, in the present study, in
order to clarify the relationship between the volume of CSF drainage
and the occurrence of RIH, we measured the postoperative volume of
blood and CSF drainage.
Figure 1
Figure 1
Remote intracranial hemorrhage in the cerebrum and cerebellum.
A) Brain computed tomogram of a 75-year-old male with ossification of the
ligamentum flavum at C7-T1. Small, subdural hemorrhage is detected in the
right cerebrum (arrow). B) Brain magnetic resonance image of a 48-yearold
female with ossification of the posterior longitudinal ligament in the
thoracic spine. Intraparenchymal bleeding is detected in the left cerebellar
hemisphere (arrow).
Figure 2
Figure 2
A 56-year-old female patient with intradural extramedullary tumor.
A) Preoperative MRI. T2-weighted sagittal MRI shows a huge intradural
extramedullary tumor extending from T12 to L5. B,C) Computed tomogram
the day after surgery. Intracranial hemorrhage is seen in the right cerebellar
hemisphere (B, arrow), tentorium cerebelli, and the left temporal lobe (B, C,
arrows).
Materials and Methods
Patient population
Between May 2007 and April 2016, a total of 691patients
underwent spinal surgeries in our department. Among these, 175
patients had durotomy or dural tear, which was confirmed in directly
findings during surgery. The demographic data of those patients are
shown in Table 1. These patients were the subjects of this study. After
durotomy or dural tear, the opened dura mater is closed by side-toside
suture or using an artificial dura with a 6-0 nylon suture as tight
as possible. Then, the closed dura is augmented by fibrin glue. Since
2008, an absorbable polyglycolic acid sheet (Neoveil®, Gunze, Kyoto,
Japan) is also used for augmentation.
Before closing the surgical wound, a relatively low-suction
drainage system, which produces negative suction pressure with a bag
(J-VAC®, made by Ethicon, Inc, Cincinnati, OH, USA), was put in the
epidural space for prevention of postoperative epidural hematoma [9-
12]. Pressure in this system can be controlled based on the height of
the drainage bag and we changed the height to maintain the drainage
volume ≤ 200-240 ml/day, postoperatively when the drainage showed
obvious serous bloody condition based on the previous reports [3,5].
The tube was removed after the drainage became obvious CSF-like
condition or the drainage volume was ≤ 50-100 ml/day.
Methods
During this study period, all patients with durotomy or dural
tear directly confirmed during surgerywere evaluated with brain
Computed Tomography (CT) on the day after surgery, regardless of
brain symptoms. The drainage volume till it was removed was also
recorded. Using these data, we first calculated the incidence of RIH.
When there were patients with RIH, the size of suction tube, location
of RIH, and prognosis of the patients with RIH were assessed. Then,
the drainage volume with and without RIH was calculated and
compared. Statistical analysis was performed with Mann-Whitney
test. P values of <0.05 were considered statistically significant.
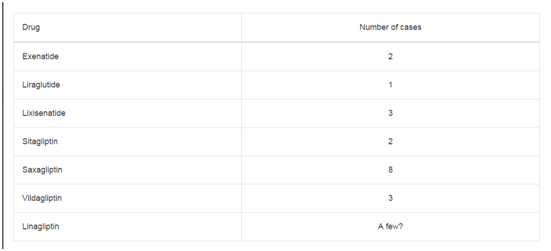
Table 1
Results
In total, three patients were affected by RIH between 2007
and 2016; all of these had durotomy or dural tear and the onset or
detection of RIH was within 24 hr postoperatively. Two patients were
asymptomatic. The incidence of RIH among all spinal surgery patients
was 0.4% (3/691); that among patients with durotomy or dural tear
was 1.7% (3/175). The diameter of the suction drainage system was 5
mm in two patients and 3.3 mm in one. In four patients, CSF drainage
from the lumbar spine was performed to reduce drainage volume
from the surgical site for dural repair but they did not show RIH.
The total and 24-hr drainage volumes of the patients with versus
without RIH after durotomy or dural tear are shown in Table 2. Both
drainage volumes of the patients with RIH were significantly larger
than those without RIH and the latter indicated stronger significant
relationship with a p value of 0.003.
Detailed data from the three patients with RIH are shown in
Table 3. One of these patients had spinal cord tumor and the two
others had ossification of the posterior longitudinal ligament or the
ligamentum flavum. One patient showed acute encephalopathy with
hydrocephalus such as headache and consciousness disturbance 12
hr after surgery. Other two patients were asymptomatic without
hydrocephalus. RIH was detected in the cerebrum alone in one
patient (Figure 1A), in both the cerebrum and cerebellum in one
patient, and in the cerebellum alone in one patient (Figure 1B).
Intraparenchymal bleeding was detected in two patients, whereas
subdural bleeding was seen in one. One patient with hydrocephalus
was treated conservatively by neurosurgeons and the other two
asymptomatic patients were just followed up regularly by brain CT.
Table 2
Case Presentation
A 56-year-old woman complained of severe bilateral leg pain and numbness with severe gait disturbance caused by a huge intradural extramedullary tumor extending from T12 to L5 (Figure 2A). The tumor was removed through T10-S1 laminectomy and durotomy. After tumor removal, the opened dura mater was closed using an artificial dura with fibrin glue. Because of the relatively high intra operative blood loss (763 ml), 5 mm-diameter suction drainage was placed before surgical wound closure for prevention of the postoperative epidural hematoma. The histological diagnosis was neurinoma. Twelve hours after surgery, the patient showed consciousness disturbance and we immediately removed the drainage tube. CT examination revealed intracranial hemorrhage in the right cerebellar hemisphere, tentorium cerebelli, and the left temporal lobe (Figures 2B and 2C). We consulted neurosurgeons in our hospital. The patient was treated conservatively with Glyceol (400 ml/day) and nicardipine hydrochloride to maintain the blood pressure between 100 and 120 mmHg. Her consciousness was gradually recovered 2 days after the onset of symptoms. Seventeen days after the onset, her brain symptoms such as disturbance of consciousness and dysphasia had completely recovered. She was moved to the ordinary program for rehabilitation after spinal cord tumor and 110 days post operatively, she could walk with crutches and discharged from our hospital.
Discussion
RIH is a potentially lethal complication associated with spinal
surgery that has just been increasingly recognized by spine surgeons
in recent years [2,13]. However, few reports have described the
incidence of RIH related to spinal surgery. In the most recent
systematic review [13], 57 cases of RIH after spinal procedures were
reported; the male/female ratio in that review was 23/34 and the
average age at surgery was 58 years (range, 23-85 years). The most
common pathology was degenerative spinal disease (60%), followed
by spinal cord tumor (21%). The most commonly affected spinal
level was lumbosacral (60%), followed by cervical (25%). The review
reported a lower incidence of RIH after spinal surgery than that
reported after supratentorial craniotomies, which is approximately
0.08% to 0.6%, however it did not indicate the exact incidence of
it. Here, we calculated it at our institution during the 9 years of the
study was 0.4% of all spine surgeries and 1.7% of those with durotomy
or dural tear. In our institution, approximately 80% of the patients
with durotomy or dural tear needed to open the dura mater to treat
the intradural lesions such as spinal cord tumor and syringomyelia
and therefore, the number of patients with durotomy or dural tear
were larger than usual. In such situation, RIH may not be as rare as
expected.
RIH can occur at various locations and can be of different types
[3,13]. The recent review cited above found 43% of reported RIH
occurred in the cerebellum, 38% were in the cerebrum, and 20%
were in both [13]. Various types of bleeding have also been reported:
subarachnoid, intraparenchymal, and subdural [3]. In this series, RIH
was detected in the cerebellum only in one patient while the other
two patients also had cerebrum bleeding. One patient had subdural
hemorrhage in the cerebrum. Actually, it occurred at various locations
with various types.
The exact mechanism of RIH after spinal surgery remains
uncertain. Intracranial hypotension caused by CSF leakage may
lead to enlargement of the dural venous sinuses and caudal brain
displacement. This displacement may create tension on enlarged
venous sinuses and predispose to venous tears. Intracranial
hypotension may stretch and tear large cortical veins crossing the
dural space. Reflex vasodilatation in response to pressure on the
dura, veins, and dural sinuses by the caudally displaced brain may
also increase the risk of subdural bleeding [3,4,14,15]. Cerebellar
involvement is most frequent and is likely related to sagging of
the cerebellum into the foramen magna after caudal displacement
[3,4,14,15].
The volume of CSF drainage is closely related to the development
of RIH [3,16]. Particularly, a sudden, large volume of CSF drainage is
likely related to RIH, as suggested by Golden JB in the “Comments”
to the article by Chadduck, the first report of RIH complicating
cervical laminectomy [1]. In our series, both total and 24-hr drainage
volumes were significantly different between the patients with versus
without RIH, and the latter showed more close relationship with
RIH occurrence. To reduce the risk of RIH by lumbar CSF drainage
after thoracoabdominal aortic repair, a drainage volume of ≤ 10 mL
in any 1-hr period was recommended by Leyvi in 2005 [17]; the
Nonprofit Organization Japanese Society of Education for Physicians
and Trainees in Intensive Care recommends a rate of ≤ 30 mL per 2
hr. The control of CSF drainage volume should be very important
to prevent the occurrence of RIH although the volume of CSF leak
during surgery cannot be controlled.
Postoperative epidural hematoma is another severe complication
in spinal surgery [18]. It is generally recommended in Japan to
use wound drainage after spinal surgery in order to prevent this
complication [19] although its effect has been reported to be
controversial [9-12,19,20]. If a wound drainage system were not used,
the discharge volume from the surgical site may decrease, whereas
the risk of postoperative epidural hematoma may increase. The
platelet reactivity and thrombolytic status of Japanese population
are somewhat different from western population [21], which may
be the reason that Japanese spine surgeons are more nervous of
postoperative epidural hematoma.
In the spinal surgery with durotomy or dural rupture, the
postoperative drainage volume should be further difficult to be
decided compared with lumbar CSF drainage after thoracoabdominal
aortic repair since each case has different conditions of bleeding
during and after surgery. If it is too restricted, spinal epidural
hematoma may occur while if it is too much, RIH may occur. Thus,
the optimal volume of drainage per hour is uncertain. All the patients
with RIH in our series had ≥ 736 ml/day drainage while those without
RIH had ≤ 790 ml/day. Based on our case series and review of the
literature, 500-700 ml/day, namely, 20-30 ml/hr may be reasonable
targets of drainage volume after spinal surgery with durotomy or
dural rupture. In the present study, we tried to maintain the drainage
volume ≤ 200-240 ml/day when the drainage showed obvious serous
bloody condition. However, all the patients with RIH had ≥ 736
ml/day drainage including blood, which indicates the difficulty of
controlling the drainage volume.
Now, we have performed the following strategy of treatment for
patients with durotomy or dural tear. During surgery, the opened
dura mater is water-tightly sutured if possible, and a suction drainage
system that has lower, can control negative pressure is used. Drainage
with full negative pressure is used when the drainage shows bloody
condition. The drainage volume is maintained at 20-30 ml/hr by the
height of drainage bag after it moves to serous bloody condition. The
drainage tube is removed soon after the drain properties changes
significant CSF. The patients are evaluated with brain CT the day
after surgery, regardless of brain symptoms, to diagnose RIH at an
early stage. However, it is occasionally very difficult to distinguish the
drainage condition; with blood dominant or with CSF dominant.
The present study has several limitations. Firstly, the patient
population was relatively small andthe study period was restricted,
which may result in the relatively high incidence of RIH after
durotomy or dural rupture. RIH appears to be a rare event and
therefore the sample size would need to be larger to draw meaningful
conclusions. Secondly, the volume of CSF leakage during surgery
cannot be measured as mentioned before since intraoperative suction
includes both blood and CSF. We cannot measure CSF and blood
individually. Thirdly, we also could not evaluate patients with occult
dural tear. It is likely that there were patients with dural tears not
confirmed during surgery. Finally, we evaluated the patients by
CT only once on the day after surgery because of the problem of
radiation exposurealthough no patients showed brain symptoms
>24 hr postoperatively. Despite these limitations, we did establish
the incidence of RIH and the possible relationship between RIH and
volume of drainage after surgery in the present study.
Table 3
Conclusion
The incidence of RIH in this study was higher than expected: 0.4% of all spine surgeries and 1.7% of those with durotomy or dural tear in our institution. RIH was closely related to CSF drainage volume, in particular, with large volume loss within a short time. Spine surgeons should be well aware of this complication and should know how to control drainage volume after spinal surgery.
Authors Contributions
Aizawa gad full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Aizawa, Ozawa and Itoi. Acquisition or interpretation of data: Aizawa, Ozawa, Ashina, Hashimoto, Kanno, Eto. Draft of the manuscript: Aizawa, Ozawa, Itoi. Study supervision: Itoi.
Compliance with Ethical Standards
The study protocol was approved by the Ethics Committee of Tohoku University Hospital (2015-1-766). Written informed consent was obtained from all included patients.
References
- Chadduck WM. Cerebellar hemorrhage complicating cervical laminectomy. Neurosurgery. 1981;9(2):185-9.
- Nam TK, Park SW, Min BK, Hwang SN. Remote cerebellar hemorrhage after lumbar spinal surgery. J Korean Neurosurg Soc. 2009;46(5):501-4.
- Estrera AL, Sheinbaum R, Miller CC, Azizzadeh A, Walkes JC, Lee TY, et al. Cerebrospinal fluid drainage during thoracic aortic repair: safety and current management. Ann Thorac Surg. 2009;88(1):9-15.
- Wynn MM, Mell MW, Tefera G, Hoch JR, Acher CW. Complications of spinal fluid drainage in thoracoabdominal aortic aneurysm repair: a report of 486 patients treated from 1987 to 2008. J Vasc Surg. 2009;49(1):29-34.
- Fedorow CA, Moon MC, Mutch WA, Grocott HP. Lumbar cerebrospinal fluid drainage for thoracoabdominal aortic surgery: rationale and practical considerations for management. Anesth Analg. 2010;111(1):46-58.
- Aizawa T, Sato T, Sasaki H, Kusakabe T, Morozumi N, Kokubun S. Thoracic myelopathy caused by ossification of the ligamentum flavum: clinical features and surgical results in the Japanese population. J Neurosurg Spine. 2006;5(6):514-9.
- Brockmann MA, Groden C. Remote cerebellar hemorrhage: a review. Cerebellum. 2006;5(1):64-8.
- Pham MH, Tuchman A, Platt A, Hseih PC. Intracranial complications associated with spinal surgery. Eur Spine J. 2016;25(3):888-94.
- Bonfield CM, Shabani HK, Kanumba ES, Ellegala DB, Nicholas J. The use of IV-tubing as a closed-suction drainage system during neurosurgical cases in Tanzania. Surg Neurol Int. 2013;4:76.
- Zijlmans JL, Buis DR, Verbaan D, Vandertop WP. Wound drains in non-complex lumbar surgery: a systematic review. Bone Joint J. 2016;98-B(7):984-9.
- Mirzai H, Eminoglu M, Orguc S. Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Dis Techniq. 2006;19(3):171-7.
- Nanba T, Ueno M, Saito W, Imura T, Inoue G, Nakazawa T, et al. Comparison of drainage tubes for closed suction drainage following spinal surgery: a prospective, randomized, clinical study. J Spine Res. 2014;5:166-71.
- Sturiale CL, Rossetto M, Ermani M, Baro V, Volpin F, Milanese L, et al. Remote cerebellar hemorrhage after spinal procedures (part 2): a systematic review. Neurosurg Rev. 2016;39(3):369-76.
- De Noronha RJ, Sharrack B, Hadjivassiliou M, Romanowski CA. Subdural haematoma: a potentially serious consequence of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 2003;74(6):752-5.
- Kelsaka E, Sarihasan B, Baris S, Tur A. Subdural hematoma as a late complication of spinal anesthesia. J Neurosurg Anesthesiol. 2003;15(1):47-9.
- Dardik A, Perler BA, Roseborough GS, Williams GM. Subdural hematoma after thoracoabdominal aortic aneurysm repair: an undererported complication of spinal fluid drainage? J Vasc Surg. 2002;36(1):47-50.
- Leyvi G, Ramachandran S, Wasnick JD, Plestis K, Cheeung AT, Drenger B. Case 3--2005 risk and benefits of cerebrospinal fluid drainage during thoracoabdominal aortic aneurysm surgery. J Cardiothorac Vasc Anesth. 2005;19(3):392-9.
- Al-Mutair A, Bednar DA. Spinal epidural hematoma. J American Academy of Orthopaedic Surgeons. 2010;18(8):494-502.
- Schroeder GD, Kurd MF, Kepler CK, Arnold PM, Vaccaro AR. Postoperative epidural hematomas in the lumbar spine. J Spinal Disord Tech. 2015;28(9):313-8.
- Hosono N, Kaito T, Makino T, Mukai Y, Miwa T, Fuji T. Does closed wound drainage really prevent epidural hematoma after lumbar surgery? Investigation upon postoperative magnetic resonance images. Rinsho Seikei Geka. 2009;44(4):397-402.
- Gorog DA, Yamamoto J, Saraf S, Ishii H, Ijiri Y, Ikaguri H, et al. First direct comparison of platelet reactivity and thrombolytic status between Japanese and Western volunteers: possible relationship to the “Japanese paradox”. Int J Cardiol. 2011;152(1):43-8.