Case Report
Laparoscopic Dorfundoplication Plus Roux-En-Y Diversion for Intractable Duodenogastroesophageal Reflux after Billroth Reconstruction
Hu Z-W1, Wang Z-G1,2, Yan C2, Tian S-R1, Deng C-R1 and Wu J-M1*
1Department of Gastroesophageal Reflux Disease, PLA Rocket Force General Hospital, China
2Department of Vascular Surgery, Xuanwu Hospital of Capital Medical University, China
*Corresponding author: Ji-Min Wu, Department of Gastroesophageal Reflux Disease, PLA Rocket Force General Hospital, No. 16 Xinwai Street, Xicheng District, Beijing, 100088, China
Published: 31 May 2016
Cite this article as: Hu Z-W, Wang Z-G, Yan C, Tian S-R,
Deng C-R, Wu J-M. Laparoscopic
Dorfundoplication Plus RouxEn-Y
Diversion for Intractable
Duodenogastroesophageal Reflux after
Billroth Reconstruction. Clin Surg. 2016;
1: 1015.
Abstract
Background: Distalgastrectomy with Billroth I or II reconstruction may cause
duodenogastroesophageal reflux and result in severe digestive even respiratory symptoms
or complications, which are often refractory to medical management, then laparoscopic
Dorfundoplication plus Roux-en-Y diversion can be selected.
Methods:Two patients with Billroth I and four patients with Billroth II had such correction for
intractable postoperative duodenogastroesophageal reflux. Patient clinical and operative data were
collected, then followed up for 1 year to 6 years.
Results: There was no mortality and morbidity after the reoperation. 5 patients had excellent symptomatic improvement and 1 not well improved. 2 patients stopped medication and 4 patients reduced medication.
Conclusions: Laparoscopic Dorfundoplication plus Roux-en-Y diversion can be an effective procedure to correct medically refractory duodenogastroesophageal reflux after Billroth I and II reconstruction, both digestive symptoms and associated respiratory symptom can be resolved after this procedure.
Keywords: Billrothreconstruction; Gastroesophageal reflux; Duodenogastroesophageal reflux;Fundoplication; Roux-en-Y diversion
Introduction
Billroth I or II anastomosis is mostly applied for distal gastrectomy. However reflux of duodenal contents into remnant stomach even esophagus and extra-esophagus can be a challenging problem after the procedure. The erosive duodenal mixed with gastric fluid is much harmful to the end organ mucosa causing severe digestive even respiratory symptoms or complications [1,2]. The main medication for gastroesophageal reflux disease (GERD), often a proton pump inhibitor (PPI), is often found to have limited effect for duodenogastroesophageal reflux (DGER) [3]. Laparoscopic fundoplication has been proved highly effective and becoming a standard antireflux procedure for GERD [4], however, a fundoplication may not sufficient to stop DGER, so we added Roux-en-Y diversion to the procedure. The purpose of this report is to describe outcome of laparoscopic Dorfundoplication plus Roux-en-Y diversion in six patients with intractable duodenogastroesophageal reflux after BillrothI and II reconstruction.
Case Presentation
From 2009 to 2014, two Patients with Billroth I and four patients with Billroth II reconstruction underwent laparoscopic Dorfondoplication plus Roux-en-Y diversion for intractable postoperative
DGER in Department of Gastroesophageal Reflux Disease of the Second Artillery General Hospital.
The study was carried out with the approval of the Ethics Committee of the Second Artillery General
Hospital. Written informed consent for participation in the study was obtained from the patients.
Laparoscopic Dorfondoplication plus a 40-cm Roux-limb Roux-en-Y diversion were carried
out as descripted in other studies [5,6] with revision (Figure 1). The patients’ demographics, DGER
evaluations and reoperation outcomes of the patientswere documented. The patients were followed
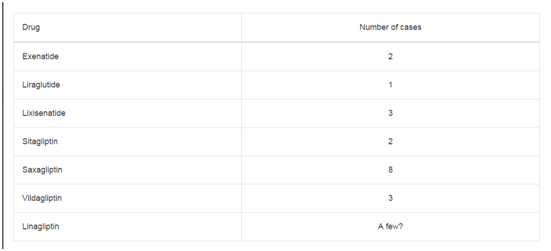
up for 1 to 6 years. There was no mortality and morbidity after the reoperation. 60-100% reduction of the DGER symptoms achieved in 5 of the 6 patients, but only one not well improved. 2 patients stopped medication and 4 patients reduced medication (Table 1).
Table 1
Case 1
This 44-year-old woman underwent distal gastrectomy with
Billroth I reconstruction forgastric cancer 18 years ago. Three
years after the gastrectomy, the patient had daily symptom of acid
regurgitation, heartburn, belch, bloating and vomit, she tried PPIs
and kinetic agents without remission. The symptoms worsened with
the occurrence of epigastric pain, and frequent bilious vomiting due
to exacerbation of the symptoms. Traditional Chinese medicine was
added to the medication formula, but still in vain. She was diagnosed
as DGER and received laparoscopic Dorfondoplication plus Rouxen-Y
diversion in our department December, 2009. During 6-year
follow-up after the procedure, herbilious vomiting disappeared, acid
regurgitation, heartburn, belch, bloating and epigastric pain were
significantly relieved (reported of 70-80% reduction). Hydrotalcite
and Omeprazole were still intermittently consumed. The patient was
satisfied with the outcome.
Case 2
This was a 53-year-old man who represented as chronic
epigastric painbefore he underwent distal gastrectomy with Billroth
I reconstruction for gastric atypical hyperplasia 2 years ago. Not
only the epigastric pain had no improvement but also the patient
developed the symptoms of intermittent chest pain, sore throat,
nausea and vomiting stomach contents and bile after the procedure.
Although high dose of PPIs and bile acid-binding agents were given to
him in many hospitals, the symptoms still worsened. The symptoms also caused sleep and diet disorders, the patient had 30 kg weight loss
in the two years. He also received laparoscopic hiatal hernia repair,
Dorfondoplication and Roux-en-Y diversion in our department
August, 2012. During 3-year follow-up after the surgery, the patient
reported no nausea and vomiting, significantly relief of chest pain,
sore throat and epigastric pain (of 60-80% reduction). Although he
still had dyspepsia and occasionally needed almagate suspension after
the procedure, he was very satisfied with the therapy.
Case 3
This 76-year-old man had distal gastrectomy with Billroth II
reconstruction for gastro duodenal ulcer 34 years ago. 3 years ago
he complained of daily severe acid reflux, heartburn and bitter taste
in the mouth. The symptoms was much severer after lying down at
night, he was frequently waken up due to chocking of large volume of
refluxing acid and bitter fluid in mouth, nasal and airway, and he was
hospitalized for aspiration pneumonia 7 times during the 3 years. He
had to strictly follow diet control and elevates the head of bed adding
to high dose of PPIs and bile acid-binding agents only to partially
reduce the symptoms. He received laproscopic Dorfondoplication and
Roux-en-Y diversion October, 2010. During 5-year follow-up after
the reoperation, his nocturnal chocking during sleep disappeared and
sleeping became normal, he only had occasionally mild acid reflux,
heartburn and bitter taste in the mouth (of 80% reduction) without
medication. He still had poor appetite, but satisfied with the therapy.
Case 4
The patient was a 67-year-old woman, she had intermittent
epigastric pain, andvomiting of stomach contents and bile after distal
gastrectomy with Billroth II reconstruction for Gastric ulcer 30 years
ago. 1 year ago, the symptoms worsened and the patient developed
the symptoms of daily regurgitation, heartburn, and bitter taste in
the mouth, unhealed multiple ulcers of mouth and tongue, globus
sensation and throat tightness with 8 kg weight loss. PPIs, bile acidbinding
agents and kinetic agents are given, the patients only had
partial and wearing off response. He also received reoperation in our
department June, 2012. During 3-year follow-up after the procedure,
her vomiting, regurgitation, heartburn, bitter taste in the mouth,
multiple ulcer of mouth and tongue, globus sensation and throat
tightness disappeared, and her epigastric pain became mild (of 90%
reduction). She occasionally taking digestive enzyme and hydrotalcite
to promote digestion and reduce epigastric pain. She was very satisfied
with the procedure.
Figure 1
Figure 1
Dorfundoplication plus Roux-en-Y diversion (C) for solving duodeno gastroesophageal reflux due to distal gastrectomy with Billroth I(A) or Billroth II (B).
Case 5
The patient was a 70-year-old woman, she represented as worsening epigastric pain, bitter taste in the mouth and intermittent vomiting of stomach contents and bile 3 years after distal gastrectomy with Billroth II reconstruction for gastric ulcer 8 years ago. Although she persistently took PPIs, bile acid-binding agents, kinetic agents and Traditional Chinese medicine for 3 years, her symptoms is still severe and troublesome. She underwent reoperation in our department January, 2013. During 2-year follow-up after the procedure, her bitter taste in the mouth and vomiting disappeared, however her epigastric pain had no remission. She stopped PPI and turned to have oxycodone-acetaminophen tablet 20 mg per day for reducing epigastric pain. She was not satisfied with the procedure.
Case 6
This is a 67-year-old woman, she had complained of regurgitation, belching, heartburn, chest pain, bitter taste in the mouth, bloating and vomiting bile since distal gastrectomy with Billroth II reconstruction for gastric atypical hyperplasia 25 years ago. The reflux contents often reached mouth, nose and even aspirated into the airway causing sore throat, globus sensation, hoarseness, postnasal drip, ears itching, teeth corrosion, irritating cough with large volume of phlegm. The symptom usually exacerbated in the morning and after meal. 2 years ago, the patient also developed the symptom of episodic laryngospasm, chest tightness and wheezing, and the cough and laryngospasm often attack at 2-4 o 'clock at night. She had to raise the head of a bed and underwent strict diet control adding to PPIs and kinetic agent’s therapy. She underwent reoperation in our department July, 2014. During 1-year follow-up after the procedure, most of her esophageal, ear-nose-throat and airway symptoms disappeared. The only symptom left were mild cough, chest tightness and bloating (of 80-90% reduction) without medication. Although her appetite was reduced after the reoperation, she was satisfied with the procedure.
Discussion
Distal gastrectomy will billroth I or II anastomosis is established
procedure for the treatment of peptic ulcer and gastric cancer, however there were often DGER [1,7]. All the patents in this group had sever gastric and esophageal symptoms, and 4 of the patients
also had extra-esophageal symptoms. When there isduodenogastric
reflux, the patents may represent as epigastric pain and gastritis [8,9],
as the duodenal fluid reflux reaches esophagus and extra-esophagus,
the patients may represent as typical GERD and extra-esophageal
symptoms, such as regurgitation, heartburn, globus sensation, bitter
taste in the mouth, cough, laryngospasm, asthmatic symptoms, etc
[10,11].
All the selected patient in this group only had partial or no
response to the long term medication therapy. The retrograde flow
of duodenal contents in DGER may result in weakly acidic and even
alkaline gastroesophageal reflux PPIs. Gamma-aminobutyric (GABA)
receptor agonist baclofen, bile acid-binding agents (Hydrotalcite,
cholestyramine, sucralfate, urosodeoxycholic acid), kinetic agents can
be used to reduce DGER, however all the agents had much limited
effect for DGER than typical GERD. For patients with medically
refractory symptoms reoperation may indicated [12,13].
Laparoscopic fundoplication is commonly used for resolving
persistent symptoms of heartburn and regurgitation in GERD,
especially when it is refractory to PPI treatment [4-14]. We also
applied laparoscopic fundoplication on extraesophageal symptoms
and obtained excellent outcomes in respect of ear-nose-throat
and respiratory symptoms. Surgical restoration of the anatomical
antireflux barrier at the gastroesophageal junction is a more
effective method of avoiding any type of gastroesophageal reflux
theoretically and is superior to medication therapy [10-15,16].
However a fundoplication dose not solve the duodenogastric reflux,
but a Roux-en-Y diversion dose [17]. Roux-en-Y reconstruction for
distal gastrectomy has been proven to have a lower incidence of bile
reflux, remnant gastritis and reflux esophagitis with better quality of
life after surgery [18,19]. As can be found in this study that most of
the patients had excellent gastric, esophageal and extra-esophageal
symptom control with significant medication reduction after
Dorfondoplication plus Roux-en-Y diversion.
Conclusion
Distal gastrectomy with Billroth I or II reconstruction may result in DGER and severe digestive even respiratory symptoms or complications which were often refractory to medical management. Laparoscopic or fundoplication plus Roux-en-Y diversion can be an effective procedure for medically refractory duodenogastroesophageal reflux after Billroth I and II reconstruction, both digestive symptoms and associated respiratory symptoms can be resolved after this procedure.
References
- Endo A, Okamura S, Kono N, Katsumi M. Esophageal reflux after gastrectomy: a hazard after Billroth-I subtotal gastrectomy. International surgery. 1978; 63: 52-58.
- Loffeld RJ. Reflux esophagitis in patients with partial gastrectomy and Billroth I or II reconstruction. Eur J Intern Med. 2006; 17: 175-178.
- Gasiorowska A, Navarro-Rodriguez T, Wendel C, , Krupinski E, Perry ZH, Koenig K, et al. Comparison of the degree of duodenogastroesophageal reflux and acid reflux between patients who failed to respond and those who were successfully treated with a proton pump inhibitor once daily. Am J Gastroenterol. 2009; 104: 2005-2013.
- Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD. SAGES Guidelines Committee. Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc. 2010; 24: 2647-2669.
- Raue W, Ordemann J, Jacobi CA, Menenakos C, Buchholz A, Hartmann J. Nissen versus Dor fundoplication for treatment of gastroesophageal reflux disease: a blinded randomized clinical trial. Dig Surg. 2011; 28: 80-86.
- Inokuchi M, Kojima K, Yamada H, Kato K, Hayashi M, Motoyama K, et al. Long-term outcomes of Roux-en-Y and Billroth-I reconstruction after laparoscopic distal gastrectomy. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2013; 16: 67-73.
- Dixon MF, O'Connor HJ, Axon AT, King RF, Johnston D. Reflux gastritis: distinct histopathological entity? J Clin Pathol. 1986; 39: 524-530.
- Paakkonen M, Aukee S, Syrjanen K, Mantyjarvi R. Gastritis, duodenogastric reflux and bacteriology of the gastric remnant in patients operated for peptic ulcer by Billroth I operation. Annals of clinical research. 1985; 17: 32-36.
- Graem N, Fischer AB, Hastrup N, Povlsen CO. Mucosal changes of the Billroth II resected stomach. A follow-up study of patients resected for duodenal ulcer,with special reference to gastritis, atypia and cancer. Acta pathologica et microbiologica Scandinavica Section A, Pathology. 1981; 89: 227-234.
- Wang Z, Hu Z, Wu J, Ji F, Wang H, Lai Y, et al. Insult of gastroesophageal reflux on airway: clinical significance of pharyngeal nozzle. Front Med. 2015; 9: 117-122.
- Wang ZG, Wu JM, Liu JJ, Wang LY, Lai YG, Ibrahim IM, et al. Respiratory distress resulting from gastroesophageal reflux is not asthma, but laryngotracheal irritation, spasm, even suffocation. Chin Med Sci J. 2009; 24: 130-132.
- . Richter JE. Duodenogastric Reflux-induced (Alkaline) Esophagitis. Curr Treat Options Gastroenterol. 2004; 7: 53-58.
- Turk H, Hauser B, Brecelj J, Vandenplas Y, Orel R. Effect of proton pump inhibition on acid, weakly acid and weakly alkaline gastro-esophageal reflux in children. World J Pediatr. 2013; 9: 36-41.
- Peters JH. Surgical treatment of gastroesophageal reflux disease. Gastroenterol Hepatol (N Y). 2014; 10: 247-248.
- Liang WT, Wu JN, Wang F, Hu ZW, Wang ZG, Ji T, et al. Five-year followup of a prospective study comparing laparoscopic Nissen fundoplication with Stretta radiofrequency for gastroesophageal reflux disease. Minerva chirurgica. 2014; 69: 217-223.
- Hu ZW, Wu JM, Liang WT, Wang ZG. Gastroesophageal reflux disease related asthma: From preliminary studies to clinical practice. World J Respirol 2015; 5: 58-64.
- Spisni R, Nervi M, Lijoi C, Colizzi C. [Roux loop conversion of Billroth II gastric resection complicated by alkaline reflux gastritis]. Minerva Chir. 1988; 43: 1227-1230.
- Xiong JJ, Altaf K, Javed MA, Nunes QM, Huang W, Mai G, et al. Rouxen-Y versus Billroth I reconstruction after distal gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol. 2013; 19: 1124-1134.
- Zong L, Chen P. Billroth I vs. Billroth II vs. Roux-en-Y following distal gastrectomy: a meta-analysis based on 15 studies. Hepatogastroenterology. 2011; 58: 1413-1424.