Research Article
Stenosis after Stapled Anopexy: Personal Experience and Literature Review
Italo Corsale*, Marco Rigutini, Sonia Panicucci, Domenico Frontera and Francesco Mammoliti
Department of General Surgery, Surgical Department ASL Toscana Centro, SS. Cosma e Damiano Hospital - Pescia, Italy
*Corresponding author: Italo Corsale, Department of General Surgery, Surgical Department ASL Toscana Centro, SS. Cosma e Damiano Hospital - Pescia, Italy
Published: 05 Oct, 2018
Cite this article as: Corsale I, Rigutini M, Panicucci S,
Frontera D, Mammoliti F. Stenosis after
Stapled Anopexy: Personal Experience
and Literature Review. Clin Surg. 2018;
3: 2140.
Abstract
Purpose: Post-operative stenosis following SA is a rare complication, however it can be strongly
disabling and require further treatments. Objective of the study is to identify risk factors and
procedures of treatment of stenosis after Stapled Anopexy.
Methods: 237 patients subjected to surgical resection with circular stapler for symptomatic IIIIV
degree haemorrhoids without obstructed defecation disorders. 225 cases (95%) respected the
planned follow-up conduced for one year after surgery.
Results: Stenosis was noticed in 23 patients (10.2%), 7 of which (3,1%) complained about “difficult
evacuation”. All patients reported symptom atology appearance within 60 days from surgery.
Previous rubber band ligation was referred from 7 patients (30,43%) and painful post-operative
course (VAS>6) was referred from 11 (47,82%) of the 23 that developed a stenosis. These values
appear statistically significant with p<0.05. Previous anal surgery and number of stitches applied
during surgical procedure do not appear statistically significant. Symptomatic stenosis was subjected
to cycles of outpatient progressive dilatation with remission of troubles in six cases. A woman, did
not get any advantage, was been subjected to surgical operation, removing the stapled line and
performing a new handmade sutura.
Conclusion: The stenosis that complicate Stapled Anopexy are high anal stenosis or low rectal
stenosis and they are precocious, reported within 60 days from surgery. If intense post-operative
pain occurs (VAS>6), this appears to be related to development of a symptomatic stenosis. Surgery
is avoidable in most cases and conservative treatment, as outpatient dilatations, has to be carried
out.
Keywords: Stapled hemorrhoidopexy; Stapled anopexy; Rectal stenosis; Anal stenosis
Introduction
Surgical treatment of the haemorrhoidal disease was been modified from the introduction of
the techniques encoded by Antonio Longo [1]. These procedures have progressively established
themselves and in 2010 the National Institute for Health and Clinical Excellence (NICE) carried
out a wide bibliographic research and finally recommended Stapled Anopexy (SA), with an I\A
Level of Evidence, as the better surgical technique to treat patients suffering from haemorrhoidal
symptomatology.
As a matter of fact, all the considered surveys demonstrated that SA produced - as compared to
the traditional Haemorrhoidectomy - a minor post-operative pain, a quicker recovery of the surgical
site, a faster recovery of the regular bowel activity, an early resumption of work and also a great
satisfaction of patients [2-4]. This indication is presently outstanding, as it is necessary to wait for
the updating expected by NICE for 2015.
This technique is not free from complications, however, and some of them, such as postoperative
hemorrhage, has been duly studied and deeply evaluated [5-8].
Post-operative stenosis following SA is considered a rare complication with a scarce impact on
the post-operative course of the patient: the survey of literature appears lacking in clinical research
to this purpose [9]. When stenosis occurs and is symptomatic, however, it can be strongly disabling
and require further treatments, that significantly extend the healing time [10].
We thought it was therefore proper to carry out a survey of our record of cases and compare it
with the data of the recent literature, in order to identify risk factors
(primary outcome) and treatments (secondary outcome) of stenosis
following SA.
Materials and Methods
During the period January 2010 – December 2014 we have
subjected 237 patients (113 men and 124 women with average age
of 54.6 ± 16 years) to transanal resection surgery by circular stapler,
because anal prolapse symptomatic for 3rd to 4th degree hemorrhoid
disease without symptoms of obstructed defecation.
All patients was subjected to a careful clinical-anamnestic
evaluation with proctoscopy and, in consideration of what appeared,
to a colonoscopy and/or virtual colon CT, anorectal manometry,
trans-rectal ultrasound test, Rx-defecography or Dinamic Magnetic
Resonance-defecography. Symptoms referred from the patients were
bleeding, prolapse, pruritus, soiling: no one referred for obstructed
defecation. Previous local treatments had been the following: rubber
band ligation for hemorrhoid (29), sclerotherapy (1), fistulectomy\
fistulotomy (3), sphincterotomy (2) or fissurotomy (1) for fissure.
On Table 1 we describe the characteristics of the patients enrolled.
No patient was subjected to mechanical bowel preparation, while
all of them were subjected to intravenous antibiotic prophylaxis
with Cefazolin 2 gr and Metronidazole 1.5 g and pharmacological
antitromboembolic prophylaxis (calcium heparin or natrum heparin)
and elastic compression stockings prophylaxis. Operations were
mainly carried out with spinal anaesthesia (229) and in gynaecological
position. The surgery technique followed Longo’s directions: after
introducing a dedicated Circular Anal Divaricator (CAD) the
prolapse was evaluated by the insertion and withdrawal of a gauze
swab. We have carried out a SA in 237 patients, performing a tobacco
bag (polypropylene 2/0) 4 cm over the linea dentata and resecting
the prolapse using a ppH 03 circular stapler (Ethicon Endosurgery®).
Hemostasis was carefully carried out at the end of operation by
transutural stitches (3/0 polyglycolic acid sutures) and a trans-anal
haemostatic pad (Tabotamp - Ethicon Endosurgery®). Number of
applied stitches was carefully recorded at the end of the operations.
Statistical Analysis
The statistical analysis was carried out using the Chi-square procedure (C) and the Fisher’s exact test (F) (SPSS version 21.0). Significant p values lower than 0.05 were considered.
Results
A 225 patients (95%) have respected the routine follow-up that
provides for a clinical evaluation with proctoscopy after one week
and one month from surgery and, in absence of complications, after 6
months and 1 year. Stenosis was reported when we have find a stricture
at the passage of the index finger and pediatric proctoscopy (18 mm)
at the rectal exploration, independently from the symptomatology
referred by the patient.
Surgery times have resulted to be between 18 and 40 minutes.
Each operation has been planned as one-day surgery.
At the follow up we have identified stenosis in 23 patients
(10,2%) (Stenosis Group - SG). Only 7 patients of them, 3,1% from
all performed SA, were symptomatic and reported “difficult of
evacuation”: symptomatology was always reported within 60 days
from surgery (range: 10-60 days – average: 25 days). 202 patients have
not a recto-anal stricture (Control Group - CG).
Previous rubber band ligation was referred from 7 patients
(30,43%) in the SG and from 22 (10,89%) in the CG. Such value
appears statistically significant, with p <0.05 (F: 0,016; C: 0,0080;
Odds ratio: 3,58). Likewise, out of the 7 symptomatic patients, 1
patient (14,3%) had been previously subjected to rubber band ligation
treatment: such value does not appears statistically significant (F:
0,621).
Previous anal surgery was referred from 1 patients (4,34 %) in
the SG and from 6 (2,97%) in the CG. Such value does not appears
statistically significant, with p>0.05 (F: 0,535; C: 0,13; Odds ratio:
1,48).
Number of applied stitches was 1 or 2 in 16 (69,56%) in the SG
and 156 (77,23%) in the CG, 3 or more than 3 in 7 (30,44%) in the SG
and 46 (22,77%) in the CG: such value does not appears statistically
significant, with p>0.05 (F: 0,439; C: 0,67; Odds ratio: 1,48).
11 patients (47,82%) in the SG suffered from a painful postoperative
course (VAS>6). This occurred in 6 patients (37,5%) who
did not report any disturbances from stenosis and in 5 patients being
symptomatic for stenosis (71,4%). Post-operative hyperalgesia was
however reported also in 33 patients (16,33%) of the 202 ones that have
not developed any further stenosis. Both values appear statistically
significant, with p<0.05 (F: 0,00116; C: 0,0003; Odds ratio 4,69).
We did not subject to any treatment the non-symptomatic patients,
while the ones who reported disturbances from obstruction have
been subjected to cycles of weekly progressive outpatient dilatation.
In six cases, we obtained a complete remission of disturbances with
six-eight applications. A woman, did not get any advantage, was
been subjected to surgical operation, removing the stapled line and
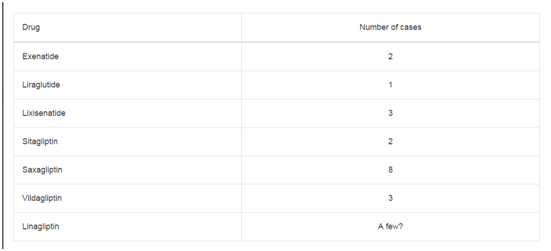
performing a new handmade sutura. Results are shown on Table 2.
Table 1
Discussion
Stenosis following surgery treatment of the hemorrhoidal disease
is a well-known clinical condition that complicates the post-operative
course in 3% to 8.5% of the patients undergone to hemorrhoidectomy
with open or closed technique (Milligan and Morgan, Ferguson,
Parks..): in these cases a stenotic scar developing and is located at
the medium or low anal canal [11,12]. The SA technique encoded by
Longo, moving the surgery action by 3 cm over the linea dentata, play
at the level of the lower rectum\higher anal canal, creating, if that
occurs, a stenosis with different characteristics. In accordance with
the Milsom’s classification of post-operative stenosis, this should be
the case of high anal stenosis, but most Authors, - and we agree with
them - believe that these should be considered lower rectal stenosis,
as they are subsequent to the resection of the rectal wall [3,13-15].
Also the classification of the stenosis degree is controversial, as it
clearly appears that it is not possible to adopt the classification of the
anal stenosis (possibility of entering the index finger for the digital
exploration) or rectal stenosis after a full-thickness anastomosis
(possibility of crossing by the sigmoidoscopy). If this complication
occurs after SA, this must be defined as “a chronic stricture of the
rectal lumen that causes signs or symptoms of complete or partial
obstruction” [3].
On this remark, it is evident how difficult it is to evaluate its real
incidence, as it varies from 0% to 8% in the surveys that we have
analyzed [16-23].
Different factors have been considered as elements favoring the
development of stenosis after SA. There is an attractive theory that
stenosis develops as result of micro-dehiscences of the suture line,
followed by a submucosa phlogosis and the subsequent formation
of retractile scar tissue [10,24]. Certainly, stenosis can be caused by
the incorrect execution of the suture line, too low and\or with a wide
resection of hemorrhoidal tissue, or asymmetrical, or too deep, or
rather at full thickness [7,24-26].
In 2006 Yao et al. [14], analyzing his personal experience,
identified in the previous hemorrhoid sclerosing treatment an
important risk factor for post operative stenosis, while he did not
report any impact by previous rectal-anal operations. These showed
however a significant value of p (<0.01) in the survey carried out by
Petersen in 2004 [3].
Finally, in 2008 Chew proposed a singular explanation of the
development of the stricture, relating it to the formation of an
exceeding anastomotic scar, similar to the one formed in the keloid
scars: that would create a hypertrophic fibrous circumferential cord,
overflowing from the linear edges [27].
It is moreover necessary to mention the unlucky occurrence of
a tight stenosis of the lower rectum: this rare complication is related
to technical mistakes such as the missed resection of the purse string
suture, the wrong positioning of the purse itself or an internal rectal
prolapse included in the purse and catched by the wrongly inclined
stapler [6,28-33].
Most stenosis, as significantly noticed in our experience, is
evidenced in the first four months from surgery, and both the
precocious and the later stenosis are rare [6]. Sex does not seem to be
a factor favoring the occurrence of stenosis [3].
The literature is poor in guidelines for the treatment of stenosis after
resective anal surgery with stapler [7]. Common sense suggests that
for all patients who report difficult evacuation after SA treatments, it
is necessary to make sure that there is no muscular functional stenosis
or a residual prolapse, and that the stricture is related to the scar. The
following treatment has to be adjusted to the length and diameter
of stenosis and its distance from the anal edge [25]. Most literature
agrees that the best and most satisfactory therapy is the progressive
dilatation connected to a proper hygienic-dietetic treatment (6,10):
dilatation can also be carried out with sedo-analgesia, in an outpatient
centre or at home, in one session or, as more often necessary, with
repeated cycles: this treatment must always be carefully conduced, in
order to avoid serious complications [34], and successful is reported
in over 95% of the cases [3]. Surgery - as also demonstrated by our
experience - is unavoidable in only 1.4% of postoperative stenosis.
The literature reports many and various surgical procedures, often
similar to that applied to colonic stricture. Expansion anoplasty is
widely employed for postoperative stenosis by Milligan and Morgan
and can be useful in strictures localized at the anoderma level, that
are consequences of incorrect “hemorrhoid resections” carried out
with circular stapler. In 2003, Garcea proposed the partial or total
resection of the scar followed by a manual adjustment of anastomosis.
The Re-Stapling method, perhaps helped by opening of stenosis with
a linear stapler, is the same one as used in colon-rectal anastomosis:
there is not a real evaluation in the colon-proctological surgery but
it undoubtedly opens up interesting consideration [35-40]. Most
Authors considering trans-anal stricturoplasty (interruption of
the fibrous pad in three-four points followed by re-adjustment of
the rectal lumen) the technique of reference in this postoperative
complication: it is safe and effective and, above all, it permits a daysurgery
treatment without giving any discomfort to the patient [3,25].
Considering these uncertainties, we believe that the gold standard
of the stenosis treatment is its prevention. To this purpose, we think
it is appropriate to follow a careful surgery procedure, correctly
preparing a uniform and symmetric suture line at 3 cm to 4 cm
over the linea dentate [7] and carefully follow the patient’s course,
placing particular attention to a possible intense post-operative pain
(VAS>6). This must lead you to suspect a micro-dehiscence and, as
such, must be treated with antibiotic therapy (3,14).
As a matter of fact, both in the survey carried out by Petersen
in 2004 [3] and in the one by Yao in 2006 [14], and as significantly
noticed in our experience, this symptom was connected to the
development of stenosis with significant values of p (p<0.003 and
p<0.01).
Therefore, in opposition to the statements of NLG about
antibiotic prophylaxis, where they support its uselessness in the
hemorrhoidectomy (1 A Level of Evidence), we think that the
trans-anal resection surgery, even if carried out for hemorrhoid
symptomatology, should be considered at the same level as the
colon-rectal resection surgery and, as such, managed with a proper
prophyilaxis.
Table 2
Conclusion
Stenosis is a possible complication, even if not a frequent one, after SA. It is a singular clinical situation that has no similar examples in proctological surgery: as a matter of fact, it is a rectal stricture that occurs after trans-anal surgery in absence of preparation of the perirectal tissues. In most cases conservative therapy is the only treatment, but 1.4% of patients’ needs surgery correction. There are no certain prevention factors, but it is surely appropriate to follow a scrupulous surgical technique by executing a correct, uniform and symmetric suture line, 3 cm to 4 cm over the linea dentata. It is moreover important to carefully follow the patient’s course. The presence of intense post-operative pain, probably also caused by anastomosis micro-dehiscence, should make you fear a successive development of stenosis.
References
- Longo A: Treatment for haemorroidal disease by reduction of mucosal and haemorrhoidal prolapse with a circular-suturing device: a new procedure. In: Proceedings of the sixth world congress of endoscopic surgery. Monduzzi Editori, Roma: 1998;777-784.
- Avgoustou C, Belegris C, Papazoglou A, Kotsalis G, Penlidis P. Evaluation of stapled hemorrhoidopexy for hemorrhoidal disease: 14-year experience from 800 cases. Minerva Chir. 2014;69(3):155-66.
- Petersen S, Hellmich G, Schumann D, Schuster A, Ludwig K. Early rectal stenosis following stapled rectal mucosectomy for hemorrhoids. BMC Surg. 2004;4:6.
- Petersen S, Jongen J, Schwenk W. Agraffectomy after low rectal stapling procedures for hemorrhoids and rectocele. Tech Coloproctol. 2011;15(3):259-64.
- Naldini G. Serious unconventional complications of surgery with stapler for haemorrhoidal prolapse and obstructed defaecation because of rectocoele and rectal intussusception. Colorect Dis. 2011;13(3):323-7.
- Pescatori M, Gagliardi G. Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol. 2008;12:7-19.
- Grigoropoulos P, Kalles V, Papapanagiotou I, Mekras A, Argyrou A, Papageorgiou K, et al. Early and late complications of stapled haemorrhoidopexy: a 6-year experience from a single surgical clinic. Tech Coloproctol. 2011;15(1):S79-81.
- Maw A, Eu KW, Seow-Choen F. Retroperitoneal sepsis complicating stapled hemorrhoidectomy: report of a case and review of the literature. Dis Colon Rectum. 2002;45:826-8.
- Lehur PA, Gravie JF, Meurette G. Circular stapled anopexy for hemorrhoidal disease: results. Colorectal Disease. 2001;3:374-9.
- Brisinda G, Vanella S, Cadeddu F, Marniga G, Mazzeo P, Brandara F, et al. Surgical treatment of anal stenosis. World J Gastroenterol. 2009;15(16):1921-8.
- Papillon M, Arnaud JP, Descottes B, Gravie JF, Huten X, De Manzini N. [Treatment of hemorrhoids with the Longo technique. Preliminary results of a prospective study on 94 cases]. Chirurgie. 1999;124(6):666-9.
- Giordano P, Gravante G, Sorge R, Ovens L, Nastro P. Long-term outcomes of stapled hemorrhoidopexy vs conventional hemorrhoidectomy: a meta-analysis of randomized controlled trials. Arch Surg. 2009;144(3):266-72.
- Milsom JW, Mazier WP. Classification and management of postsurgical anal stenosis. Surg Gynecol Obstet. 1986;163(1):60-4.
- Yao L, Zhong Y, Xu J, Xu M, Zhou P. Rectal stenosis after procedures for prolapse and hemorrhoids (PPH)--a report from China. World J Surg. 2006;30(7):1311-5.
- Mehigan BJ, Monson JR, Hartley JE. Stapling procedure for haemorrhoids versus Milligan-Morgan haemorrhoidectomy: randomised controlled trial. Lancet. 2000;355:782-5.
- Pavlidis T, Papaziogas B, Souparis A, Patsas A, Koutelidakis I, Papaziogas T. Modern stapled Longo procedure vs. Conventional Milligan-Morgan hemorrhoidectomy: a randomized controlled trial. Int J Colorectal Dis. 2002;17:50-53.
- Singer MA, Cintron JR, Fleshman JW, Chaudhry V, Birnbaum EH, Read TE, et al. Early experience with stapled hemorrhoidectomy in the United States. Dis Colon Rectum. 2002;45:360-7.
- Boccasanta P, Capretti PG, Venturi M, Cioffi U, De Simone M, Salamina G, et al. Randomised controlled trial between stapled circumferential mucosectomy and conventional circular hemorrhoidectomy in advanced hemorrhoids with external mucosal prolapse. Am J Surg. 2001;182:64-8.
- Ho YH, Cheong WK, Tsang C, Ho J, Eu KW, Tang CL, et al. Stapled hemorrhoidectomy cost and effectiveness. Randomized, controlled trial including incontinence scoring, anorectal manometry, and endoanal ultrasound assessments at up to three months. Dis Colon Rectum. 2000;43:1666-75.
- Kirsch JJ, Staude G, Herold A. The Longo and Milligan-Morgan hemorrhoidectomy. A prospective comparative study of 300 patients. Chirurgie; 2001;72:180-5.
- Ravo B, Amato A, Bianco V, Boccasanta P, Bottini C, Carriero A, et al. Complications after stapled hemorrhoidectomy: can they be prevented? Tech Coloproctol. 2002;6:83-8.
- Shalaby R, Desoky A. Randomized clinical trial of stapled versus Milligan-Morgan haemorrhoidectomy. Br J Surg. 2001;88:1049-53.
- Correa-Rovelo JM, Tellez O, Obregon L, Miranda-Gomez A, Moran S. Stapled rectal mucosectomy vs. closed hemorrhoidectomy: a randomized, clinical trial. Dis Colon Rectum. 2002;45:1367-74.
- Angelone G, Giardiello C, Prota C. Stapled hemorrhoidopexy. Complications and 2-year follow-up. Chir Ital. 2006;58(6):753-60.
- Dowden JE, Stanley JD, Moore RA. Obstructed defecation after stapled hemorrhoidopexy: a report of four cases. Am Surg. 2010;76(6):622-5.
- Katdare MV, Ricciardi R. Anal stenosis. Surg Clin North Am. 2010;90(1):137-45.
- Chew MH, Chiow A, Tang CL. Keloid formation after stapled haemorrhoidectomy causing anal stenosis: a rare complication. Tech Coloproctol. 2008;12(4):351-2.
- Cipriani S, Pescatori M. Acute rectal obstruction after PPH stapled hemorrhoidopexy. Colorectal Disc. 4:367-370.
- Mongardini M, Custureri F, Schillaci F, Leone G, Cola A, Fanello G, et al. [Rectal stenosis after stapler hemorrhoidopexy]. G Chir. 2005;26(6-7):275-7.
- Giordano P, Bradley BM, Peiris L. Obliteration of the rectal lumen after stapled hemorrhoidopexy: report of a case. Dis Colon Rectum. 2008;51:1574-6.
- Baraza W, Shorthouse A, Brown S. Obliteration of the rectal lumen after stapled hemorrhoidopexy: report of a case. Dis Colon Rectum. 2009;52(8):1524-5.
- Vasudevan SP, Mustafa el A, Gadhvi VM, Jhaldiyal P, Saharay M. Acute intestinal obstruction following stapled haemorrhoidopexy. Colorectal Dis. 2007;9(7)9:668-9.
- Büyükaşik O, Hasdemir OA, Cöl C. Rectal lumen obliteration from stapled hemorrhoidopexy: can it be prevented? Tech Coloproctol. 2009;13(4):333-5.
- Kanellos I, Blouhos K, Demetriades H, Pramateftakis MG, Betsis D. Pneumomediastinum after dilatation of anal stricture following stapled haemorrhoidopexy. Techniques in Coloproctology. 2004;8(3):185-7.
- Sileri P, Stolfi VM, Franceschilli L, Perrone F, Patrizi L, Gaspari AL. Reinterventions for Specific Technique-Related Complications of Stapled Haemorrhoidopexy (SH): A Critical Appraisal. J Gastrointest Surg. 2008;12(11):1866-73.
- Brusciano L, Ayabaca SM, Pescatori M, Accarpio GM, Dodi G, Cavallari F, et al. Reinterventions after complicated or failed stapled hemorrhoidopexy. Dis Colon Rectum. 2004;47(11):1846-51.
- Garcea G, Sutton CD, Lloyd TD, Jameson J, Scott A, Kelly MJ. Management of benign rectal strictures. A review of present therapeutic procedures. Dis Col Rect. 2003;46:1451-60.
- Ovnat A, Peiser J, Avinoah E, Charuzi I. A new approach to rectal anastomotic stricture. Dis Colon Rectum. 1989;32(4):351-3.
- Hinton CP, Celestin LR. A new technique for excision of recurrent anastomotic strictures of the rectum. Ann R Coll Surg Engl. 1986;68(5):260-1.
- Pagni S, McLaughlin CM. Simple technique for the treatment of strictured colorectal anastomosis. Dis Colon Rectum. 1995;38:433-4.