Case Report
Left Hepatic Lobe Herniating Through Sternotomy Incision
Amer Hashim Al Ani1*, Mustafa Y Rashid Al Badra2, Sabah Al Kaisy1, Hesham Abdulmoneim,1, Hassan Abdulhakim1, Zahir Al jowher2, Eltegani Eltayieb Ahmed1 and Gada Al Khalid1
1Department of General Surgery, Sheikh Khalifa Medical City, Sheikh Khalifa General Hospital, Ajman, United Arab
Emirates
2Department of Diagnostic Radiology, Sheikh Khalifa Medical City, Sheikh Khalifa General Hospital, Ajman, United
Arab Emirates
*Corresponding author: Amer Hashim Al Ani, Department of General Surgery, Sheikh Khalifa Medical City, Sheikh Khalifa General Hospital, Ajman, United Arab Emirates
Published: 03 Aug, 2017
Cite this article as: Al Ani AH, Al Badra MYR, Al Kaisy
S, Abdulmoneim H, Abdulhakim H,
Al jowher Z, et al. Left Hepatic Lobe
Herniating Through Sternotomy
Incision. Clin Surg. 2017; 2: 1686.
Abstract
Introduction: Liver herniation through surgical incision is very rare. Moreover, it is exceptional for
the left hepatic lobe to herniate through sternotomy incision.
Presentation of the case: We present herein a 66-year-old woman admitted to ER complains about
upper abdominal pain. Abdominal CT scan showed herniation of part of left hepatic lobe through
previous sternotomy incision. Conservative measures were successful in managing her symptoms.
Discussion: Till now only few cases of liver herniation through scar of sternotomy have been
documented.
Conclusion: Although it is rare, left hepatic lobe may herniate through sternotomy incision.
Keywords: Left lobe liver; Sternotomy; Incisional hernia
Introduction
It is very rare for a liver or part of it to be involved in a hernia. Congenital and traumatic diaphragmatic hernias are the most common hernias to contain liver [1,2]. Only few cases of liver herniated through incision of sternotomy were documented in medical literatures [3]. Asymptomatic cases were treated conservatively [3], while those with symptoms were treated by surgery to repair the hernia and reduce its content (liver) [4].
Case Presentation
We report a 66-year-old women presented to ER with upper abdominal pain following heavy
meal. The pain was burning in nature, radiates to the back. Associated with nausea, there was no
vomiting, fever, chills, or itching. She noticed no changes in her bowel habit, color or consistency.
She identified a non-painful swelling protruded from her upper abdomen 2 years ago. She is
asthmatic, diabetic, had history of myocardial infarction. Three years back she had Coronary Artery
Bypass Grafting (CABG). She is on aspirin, amlodipine, frusemide, Insulin and nebulizer. She is not
smoker. Not drinking alcohol.
On examination: She was pale, not jaundiced. Her vital signs were within normal. By inspection;
there was a scar of previous sternotomy extending from the chest to upper part of abdomen. A 6 cm
× 6 cm mass was protruding from the scar. The mass was soft by palpation. It was not tender. The
rest of the abdomen was soft, apart from mild tenderness in epigastric region. Bowel sounds were
active. Laboratory tests revealed: low Hemoglobin (9.80 gm/dl), low serum iron (5.90 umol/l), high
blood sugar (7.8 mmol/l ), high blood Urea (10.70 mmol/l), low Albumin (30.0 gm/l), low serum
Calcium (2.09 mmol/l), normal T4 Free (15.82 pmol/l), low T3 Free (3.52 pmol/l), high TSH (4.64
mIU/l), high D-Dimer (1.30 mg/l), high Hemoglobin A1c (8.1%), high C reactive protein (19.9 mg/l),
normal liver function test, normal lipase and amylase. Serum electrolytes were within normal. All
the abnormal parameters were corrected. ECG, Echocardiography was done for the patient. Then
her cardiac problems were managed by the cardiologist. OGD (esophagogastroduodenoscopy)
showed reflux gastritis. This was controlled by proton pump inhibitors. Computed tomography
abdomen revealed herniation of the left lobe of the liver (Figure 1 and 2) with surrounded fat
through a large epigastric defect just below a previous sternotomy incision (Figure 3 and 4). The
herniated part appear iso-dense to the normal liver. Severe intervertebral disc generation seen with possibility of multiple disc prolapses. After two days of conservative management in hospital, her pain was relieved, her blood sugar was
controlled, and her parameters were good. She was discharged home
in a good general condition. For the next three months patient was
asymptomatic.
Figure 1
Figure 1
Plain chest X-ray showing median sternotomy closure with
interrupted stainless steel wires.
Figure 2
Figure 2
Sagittal CT scan image (arterial phase) revealed herniation of
the left lobe of the liver (white asterisk) with surrounded fat through a large
epigastric defect just below a previous sternotomy incision (white arrow).
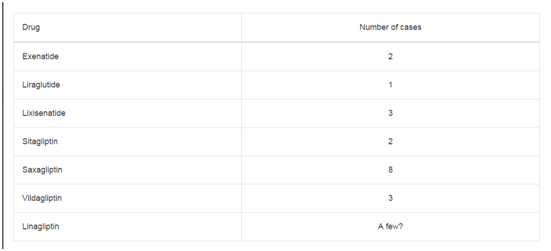
Table 1
Discussion
Liver hernia is very rare (Table 1) [1,5]. Congenital diaphragmatic
defects and blunt trauma diaphragmatic rupture are the most
common documented causes resulting in this hernia [2]. Obesity and
previous abdominal surgery are other less common causes [6]. Up
to May 2015 only three cases have been reported for liver herniation
through scar of previous of CABG surgery as in this case. Abdominal
pain, discomfort, nausea, vomiting, jaundice, dyspnea, confusion and
swelling are the most common presenting symptoms. In our case the
presenting symptom was abdominal pain. Left lobe of the liver is the
most common part of the liver to herniate through abdominal wall.
This hernia may progress to an incarcerated incisional hernia [7,8].
Median sternotomy for coronary artery bypass [3,9] (this is the surgery
in this case), midline laparotomy for trauma, intestinal obstruction,
orthotopic liver transplantation [10], open cholecystectomy [11]
and for choledochotomy to remove liver hydatid cyst [12]. Right
subcostal incision for open cholecystectomy and right flank incision via a retroperitoneal approach for nephrectomy, are the comments
operations complicated by liver hernia. Sabbah-Briffaut et al. [12]
report an entity described in neonatal period known as exclusive
hepatocele, in which the liver is part of omphalocele contents [13].
Transabdominal ultrasound, CT scan and magnetic resonance
imaging can usually appropriately determine liver as the hernia
content. CT scan confirmed left lobe of liver as a content of incisional
hernia in our case. Conservative therapy should be considered first in
these rare patients, especially asymptomatic patients and those whose
symptoms were minimal. In this case we were able to control the
symptoms with symptomatic treatment. However, surgical therapy
may be an option for patients with more severe complaints.
Figure 3
Figure 3
Axial CT scan image (venous phase) shows the herniated liver
parenchyma through the epigastric anterior abdominal wall defect, the
herniated part appear isodense to the normal liver.
Figure 4
Conclusion
Left lobe of liver rarely herniates through abdominal extension of sternotomy incision following CABG (Coronary artery bypass grafting). A CT scan can confirm the diagnosis. Conservative treatment is usually successful.
References
- Mullassery D, Baath ME, Jesudason EC, Losty PD. Value of liver herniation in prediction of outcome in fetal congenital diaphragmatic hernia: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2010;35(5):609-14.
- Kim HH, Shin YR, Kim KJ, Hwang SS, Ha HK, Byun JY, et al. Blunt traumatic rupture of the diaphragm: sonographic diagnosis. J Ultrasound Med. 1997;16(9):593-8.
- Shanbhogue A, Fasih N. Education and imaging. Hepatobiliary and pancreatic: herniation of the liver. J Gastroenterol Hepatol. 2009;24(1):170.
- Neelamraju Lakshmi H, Saini D, Om P, Bagree R. A ventral incisional hernia with herniation of the left hepatic lobe and review of the literature. BMJ Case Rep. 2015;2015.
- Ansari S, Shaikh TP, Mandhane N, Deolekar S, Karandikar S. A rare case of herniation of liver through incision of cabg: A case report and review of literature. Int J Res Med Sci. 2015;3(7):1817-9.
- Nuño-Guzmán CM, Arróniz-Jáuregui J, Espejo I, Valle-González J, Butus H, Molina-Romo A, et al. Left hepatic lobe herniation through an incisional anterior abdominal wall hernia and right adrenal myelolipoma: a case report and review of the literature. J Med Case Reports. 2012;6:4.
- Abci I, Karabulut Z, Lakadamyali H, Eldem HO. [Incarceration of the left hepatic lobe in incisional hernia: a case report]. Ulus Travma Acil Cerrahi Derg. 2005;11(2):169-71.
- Salemis NS, Nisotakis K, Gourgiotis A, Tsohataridis E. Segmental liver incarceration through a recurrent incisional lumbar hernia. Hepatobiliary Pancreat Dis Int. 2007;6(4):442-4.
- Warbrick-Smith J, Chana P, Hewes J. Herniation of the liver via an incisional abdominal wall defect. BMJ Case Rep. 2012;2012.
- Sheer TA, Runyon BA. Recurrent massive steatosis with liver herniation following transplantation. Liver Transpl. 2004;10(10):1324-5.
- Tekin F, Arslan A, Gunsar F. Herniation of the liver: an extremely rare entity. J Coll Physicians Surg Pak. 2014;24(3):S186-7.
- Sabbah-Briffaut E, Houfflin-Debarge V, Sfeir R, Devisme L, Dubos JP, Puech F, et al. Liver hernia. Prognosis and report of 11 cases. J Gynecol Obstet Biol Reprod (Paris). 2008;37(4):379-84.
- Bonatti M, Lombardo F, Vezzali N, Zamboni GA, Bonatti G. Blunt diaphragmatic lesions: Imaging findings and pitfalls. World J Radiol 2016;8(10):819-28.