Research Article
Stretching the Cardiac Donor Ischemic Time to Beyond Six Hours: What’s the Impact?
Rahul Chandola1*, Masato Mutsuga2, Colleen Norris1 and Shaohua Wang1
1Division of Cardiovascular Surgery, University of Alberta Hospital, Canada
2Department of Cardiac Surgery, Nagoya University, Japan
*Corresponding author: Rahul Chandola, Division of cardiovascular surgery, University of Alberta hospital, Edmonton, Alberta, T6G 2B7, Canada
Published: 04 Aug, 2017
Cite this article as: Chandola R, Mutsuga M, Norris C,
Wang S. Stretching the Cardiac Donor
Ischemic Time to Beyond Six Hours:
What’s the Impact?. Clin Surg. 2017;
2: 1578.
Abstract
Objective: The evidence evaluating the impact of prolonged ischemia time, in particular beyond 360
min in the adult population, on the heart transplant outcomes is limited. We sought to determine if
prolonged ischemic times beyond 360 min has any impact on the postoperative outcomes and short,
midterm and long term survival of heart transplants at University of Alberta.
Material and Method: Data was collected from the Alberta Provincial Project for Outcome
Assessment in Coronary Heart Disease (APPROACH) database. This database is a prospective data
collection registry that collects real-time data, from three hospital sites, beginning at the patient’s
referral for cardiac catheterization. Data is entered into the APPROACH registry along the patient’s
clinical trajectory. The APPROACH database is a mandatory registry for all patients in all hospitals
that provide cardiac catheterization, coronary revascularization and cardiac surgery in Alberta.
Results: Univariate analysis, identified a significant difference between PIT (prolonged ischemic
time) and MIT (moderate ischemic time) groups in 30 day (23.7% and 8.6%, p< 0.001) and 6 month
mortality (24.7% and 9.9% p< 0.001). Long term survival between groups was also significantly
different (p=0.04) between both groups. Though univariate analysis did show significant mortality
differences, when we controlled both the groups for the variables such as prior PCI, pretransplant
dialysis, pretransplant liver dysfunction, donor age and duration of cardiopulmonary bypass, there
were no significant differences in survival outcomes between the two groups (hazard ratio 1.19).
Conclusion: With the current techniques of myocardial preservation, modified reperfusion and the
detailed evaluation of recipient and donor factors on a case by case basis, donor hearts with ischemia
time greater than 6 h provide comparable postoperative outcomes and short, intermediate and long
term survival results. The prolonged ischemic times, in itself, should not be a contraindication for
transplant.
Introduction
An estimated 5.1 million Americans ≥20 years of age have heart failure. By 2030, the prevalence of HF is believed to increase by 25% [1]. The International Society for Heart and Lung Transplantation (ISHLT) registers upto 3,500-4,000 heart transplants worldwide every year. The number of transplants done annually have been quite static over last 20 years despite the growing heart failure population. The shortage of donor hearts has clearly limited the number of heart transplantations [2]. This disparity in organ (heart) demand and the ever increasing shortage of donors has led to a need to expand the donor eligibility criteria. This has led to accepting the donor organs from remote places, with the anticipated prolonged ischemic times. Although donor ischemic time’s upto 4 h - 5 h are generally acceptable, the benefits of ischemic times in excess of 240-300 min are still arguable [3]. Although many studies have analyzed the impact of long ischemic times on the adult cardiac transplant outcomes in terms of survival and graft function [3-6], these studies have been limited by a relatively small number of patients with longer ischemic time ranges. As a result, the evidence evaluating the impact of prolonged ischemia time, in particular beyond 360 min in the adult population, on the heart transplant outcomes is limited. We sought to determine if prolonged ischemic times beyond 360 min has any impact on the short, midterm and long term survival and the postoperative outcomes of heart transplants at University of Alberta.
Methods
Data was collected from the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) database. This database is a prospective
data collection registry that collects real-time data, from three
hospital sites, beginning at the patient’s referral for cardiac
catheterization. Data is entered into the APPROACH registry
along the patient’s clinical trajectory. The APPROACH database
is a mandatory registry for all patients in all hospitals that provide
cardiac catheterization, coronary revascularization and cardiac
surgery in Alberta, Canada, and a province of approximately 3.7
million people. APPROACH contains demographic data as well as
the presence or absence of previous myocardial infarction, congestive
heart failure, cerebrovascular disease, peripheral vascular disease,
chronic pulmonary disease, elevated creatinine, renal dialysis,
hyperlipidemia, hypertension, liver disease, gastrointestinal disease,
and malignancy as well as indication for revascularization, extent of
CAD, and procedural data including pre, peri- and post-operative
data. Adverse events data are also recorded in the APPROACH
database and reviewed through various hospital based morbidity and
mortality rounds. As the data in APPROACH is used for both clinical
and administrative purposes, software checks have been put into
place to ensure that there are limited missing data particularly in the
baseline characteristics of the patients in APPROACH. Furthermore,
for the purposes of research, we annually employ a data replacement
method that has been validated and ensures that the data is over 95%
complete. From this database patients are followed longitudinally for
the determination of short and long-term outcomes. For the purposes
of this study, cardiac catheterization and/or echocardiography were
used to measure EF and LVEDP.
Donor acceptance criteria
After establishment of brain death, donor was matched with
recipient for ABO blood compatibility and body weight matching.
We accept donors within 20% of the recipient weight. Prospective
human leukocyte antigen (HLA) matching was not used but the
patients with high levels of panel reactive anti-HLA antibodies
underwent a prospective cross-match. The donors are accepted
preferably under age 60, especially if long ischemic times are expected.
The echocardiogram should not reveal any structural heart disease,
shunts (except patent foramen ovale), more than mild left ventricular
hypertrophy and no significant wall motion abnormalities. Other
factors to be considered include hemodynamic stability and not more
than small to moderate doses of inotropic support. We prefer to have
coronary angiograms for patients >45 years. Coronary angiogram
should not reveal anything more than mild coronary artery disease.
The donor should not have a history of heart disease, sepsis; known
malignancy (some primary brain tumors can be accepted). Serologies
should be negative for HIV, hepatitis B (hepatitis B sAg), hepatitis C,
HTLV and syphilis.
Donor exclusion criteria
Donors with ABO incompatibility, body weight and size mismatch
and those who do not meet brain death criteria as outlined under
policies, are excluded. Other excusion criteria are HIV positivity,
Hepatitis B surface antigenemia, Hepatitis C positivity, evidence
of significant infection or sepsis, any structural cardiac deformity,
ventricular arrhythmias, more than mild coronary artery disease on
angiogram, poor left and/or right ventricular function that does not
responds to relevant inotropic, preload and after load manipulations
and/or ejection fraction < 45% or fractional shortening < 25%,
echocardiographic evidence of significant valvular abnormality,
any acute malignancy (except some primary brain tumors), carbon
monoxide poisoning as the cause of death and history of intravenous
drug use.
Graft procurement
Goal at this juncture is the effective treatment of potential cardiac
arrhythmias, hemodynamic instability, metabolic acidosis and diabetes
insipidus. Methylprednisolone 10- 15 mg/kg bolus, Triiodothyronine
(T3) 3 mcg/hr, Thyroxin (T4) 10 mcg/hr, vasopressin 0.5 - 4 units/
hr is started and titrated to keep SVR 850 - 1250. Insulin infusion is
run at 1 unit/hr and titrated to keep blood glucose levels to 120 - 180
mg/dl. Donor hearts were harvested from heart-beating, brain-dead
individuals. Donor hearts were perfused with 2 L of Celsior solution
at a constant pressure of 60 mmHg over a 7 - 10 min period and were
transported immersed in hypothermic celsior solution with normal
saline at 4 - 8 C. Biatrial technique described by Lower and Shumway
was utilized for transplantation before year 2000 and we changed to
bicaval anastomosis technique since then [5,6].
Immunosuppressive regimen
The use of routine induction therapy is the current standard of
care for all patients undergoing cardiac transplant at the University of
Alberta, with one exception: anti-HCV positive patients do not receive
induction. Primary agent used for induction is Rabbit anti-thymocyte
globulin (Thymoglobulin®) given at a dose of 0.75 mg/kg IV in 250
ml of NS via central line to run over 12 hours twice a day for 3 days.
The daily dose is continued to maintain absolute lymphocyte count
(ALC) ≤0.2x 109/L x >2 days. Tacrolimus is started every 12 h once
the renal function stabilizes with the dose to be adjusted in response
to serum drug levels. Tacrolimus is usually administered orally q 12 h
(8 am and 8 pm) beginning post-operatively when bowel sounds are
present and renal function is stable (optimally when it is approaching
baseline). The initial oral dose is 0.075 mg/kg/day administered in
two divided doses. At 0 - 3 months, tacrolimus levels are maintained
at 8-12 ug/L, at 3-6 months in the range of 6-10 ug/L and 6 months
onwards at 5-8 ug/L. Since 2000, azathioprine was replaced by
mycophenolate mofetil (MMF). Usual dose is 500-1500 mg po BID
for MMF. Individual dosage adjustments are made according to
patient response (GI tolerance) and WBC’s. Methylprednisolone
(2mg/kg) IV is given perioperatively every 12 h for 3 doses. First dose
is started within four hours of patient arrival in CVICU.
Prednisone is started at 1 mg/kg NG/PO daily, after third dose of
methylprednisolone, if bowel sounds are present. The dose is tapered
per day to achieve 0.3 mg/kg/day by 30 days post-transplant. Tapering doses of prednisone are calculated for each patient individually to
achieve the following: 1-month post-op: 0.3 mg/kg daily, 2-months
post-op: 0.2 mg/kg daily, 3-months post-op: 0.1 mg/kg daily and
further weaning to discontinue prednisone by 6 months.
Recipient exclusion criteria
Exclusion criteria for cardiac transplantation were factors
that adversely impact long-term survival (eg. cancer), increase
perioperative morbidity and mortality (eg. pulmonary hypertension,
recent pulmonary embolus, active infection), or affect a patient's
ability to care for him- or herself (eg, untreated major psychiatric
illness, recent substance abuse). Pretransplant pulmonary
hypertension, defined as greater than 6 Woods units, was also
considered to be a relative contraindication to transplantation. Many
of these comorbidities, however, are being reevaluated, given our
favorable experience in transplanting patients once perceived to be
high risk (eg. diabetics).
Statistical analysis
All pre-operative, peri-operative and post-operative categorical
variables were compared among the two groups by χ2 test for
independence, and continuous variables (age and body mass index)
were compared by one-way analysis of variance (ANOVA) with
post-hoc Bonferroni correction. Long-term survival after heart
transplantation was estimated using Kaplan-Meier actuarial log
rank statistics for the two groups. Multi-variate regression using Cox
proportional hazards modeling was used to determine independent
risk factors for death for all patients analyzed in the cohort.
Figure 1
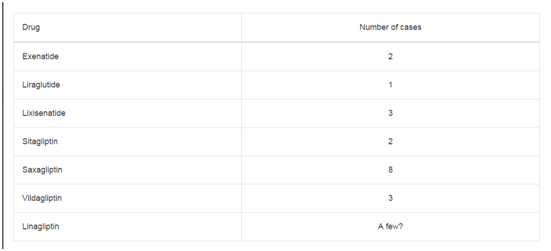
Table 1
Table 2
Table 3
Table 4
Results
From January 1992 through January 2012, 475 patients
underwent cardiac transplantation at University of Alberta hospital.
The recipients were separated into the two groups based on length of
ischemic time in minutes: group 1, moderate Ischemic Time (MIT),
120 - 359 min (n=382); group 2 prolonged Ischemic Time (PIT),
>360 min (n=93). All 475 recipients were included in the analysis,
including patients who died in the early postoperative period.
Ischemic time was defined as the interval from application of donor aortic crossclamp to release of the recipient crossclamp.
Recipient demographics
The PIT group, had 69 males (74.2%) 24 females (25.8%),
had a mean age at transplantation of 50.9 years, mean BMI at
transplantation of 29.5, and a median waiting time of 19.3 days (3.4
to 260.8 days). The MIT group, 303 males (79.3%) and 79 females
(20.7%), had a mean age at transplantation of 51.4 yrs (SD -12.8),
mean BMI at transplantation of 27.2 (SD -15.3) and a median waiting
time for an organ of 10.3 days (0.8 to 57.5 days). There were no
statistically significant differences between the groups in terms of
recipient gender, age, mean BMIs or median waiting time (Table 1).
The significant demographic differences were in terms of relatively
younger donors in the MIT group (27.5% vs. 12.2% donors < 21 years
and 23.8% vs. 37.8% donors >47 years, p value- 0.003), frequency of
prior PCI (with recipients in MIT group having a lower incidence
of previous PCI) (18.8% vs. 28.7%, p value- 0.04), PIT group having
higher number of patients who were being treated with dialysis
(16.1 vs. 5.1 p value- 0.001) and higher number of patients with liver
disease (11.8% vs. 2.5%, p value- < 0.001). As would be expected, the
PIT group had significantly longer pump times (355.4 vs. 194.8 min,
p value < 0.001) and associated cross clamp times.
Postoperative outcomes
The incidence of postoperative bleeding was significantly higher
in PIT group (13.8% vs. 7.8%, p value. 05) (Table 2). Neurological
complications were also quite higher in the PIT group (18.4% vs.
7.6%, p value- 0.002). Specifically 6.5% of the patients in PIT group
had permanent stroke as opposed to 0.8% in the MIT group (p
value- < 0.001). 2.2% patients in the PIT group had transient stroke
as compared to 0.8% in the MIT group (p value < 0.001). 3.2% of the
patients stayed in continuous coma as opposed to 0.8% of the patients
in MIT group (p value < 0.001). Incidence of sternal wound infection,
duration of ventilation, incidence of postoperative renal dysfunction,
incidence of dialysis requirement, cardiac tamponade, cardiac
rejection during primary hospitalization were similar between both
the groups.
Survival outcomes
Univariate analysis, identified a significant difference between PIT
and MIT groups in 30 day (23.7 % and 8.6%, p < 0.001) and 6 month
mortality (24.7% and 9.9% p < 0.001). Long term survival between
groups was also significantly different (p=0.04) between both groups
(Figure 1). Cox proportional hazards models were used to test the
independent effect of ischemic time on mortality while controlling
for pre, peri and post operative variables that were significantly
associated with ischemic time (Table 3).
In model 1, after adjusting for heart failure, prior PCI, Dialysis,
and liver disease, the hazard ratio was 1.5 (95% upper and lower CI
1.00 & 2.29.) (p=0.06).
In model 2, following adjustment for donor age and pump time
in minutes, the hazard ratio was 1.19 (95% upper and lower CI 0.76
& 1.85.) (p value=0.45).
Finally in model 3, we adjusted for neurological complications.
The hazard ratio was 1.13 with 95% upper and lower CI of 0.72 and
1.77(p value- 0.60).
Discussion
With the ever expanding heart failure population in need of
heart transplantation and a shortage of donor organs, cardiac
centers often have to accept organs from far off places in an effort to
increase the donor pool, leading to prolonged ischemic times. There
has been a lot of confusion in regards to effect of donor ischemic
times on transplant outcomes. Some of the studies did not find
any relationship between ischemic time and survival [7-9]. Some
multi-institutional studies, on the other hand, found early mortality
after transplantation to be affected by prolonged donor ischemic
times [10-12]. There were few other studies that found an inverse
relationship between donor ischemic times and survival outcomes
[13]. Mullen et al. from our institution compared the groups with
donor ischemic times lesser and greater than 4 h and did not find
any difference in the 30-day, 90-day or actuarial survival between
the groups [14]. The use of allografts with ischemia times greater
than 4-5 h has been reported by some investigators with prolonged
ventilation, prolonged ICU stay, prolonged hospital stay, increased
graft dysfunction, and higher morbidity and early mortality [15-20].
It was interesting to find, contrary to previous studies, there wasn’t
significant difference between the two groups in terms of need for
prolonged ventilation (40.3% in MIT vs. 46.2 %in PIT, p value- 0.30),
length of ICU stay (11.4 vs. 11.1 days, p value- 0.88) or duration of
hospital stay (26.3 vs. 26.7 days, p value- 0.92). Interestingly, the
length of inotropic support also did not differ significantly between
both the groups. The incidence of renal failure and the number of
patients requiring dialysis were also not statistically different. 30 day
biopsy-proven acute cellular rejection grade 3A or greater was not
statistically different in both the group. 15.7% of the patients in MIT
group had grade 3A or greater acute cellular rejection compared to
12.9% in the PIT group (p value- 0.50). There was a difference in the
incidence of postoperative bleeding in both the groups. We found
7.4% incidence of take backs for postoperative bleeding in MIT
group as compared to 13.8% in the PIT group (p value- 0.05). This is
possibly a result of increased cardiopulmonary bypass times in PIT
group (mean of 355.4 min vs. 194.8 minutes, p < 0.001) leading to
coagulopathy and platelet dysfunction, accounting for increased take
backs in this group. We also found a significantly high incidence of
neurological adverse events in the PIT group (18.4% vs. 7.6%, p value-
0.02). Specifically 6.5% of the patients in PIT group had permanent
stroke as opposed to 0.8% in the MIT group (p value- < 0.001). 2.2% patients in the PIT group had transient stroke as compared to 0.8%
in the MIT group (p value < 0.001). 3.2% of the patients stayed in
continuous coma as opposed to 0.8% of the patients in MIT group (p
value < 0.001). Interestingly, the majority of patients with permanent
stroke had ischemic cardiomyopathy as the etiology of heart failure. It
is known that patients with ischemic cardiomyopathy have significant
atherosclerotic disease and it is possible there was a preexisting
burden of cerebrovascular atherosclerotic disease that could have
led to increased incidence of strokes in this group as suggested by
some earlier studies [21]. We could not find any other specific
differences between the two groups of patients with strokes because
of the relatively small number of patients with permanent strokes.
On univariate analysis, survival outcomes were quite significantly
different between both the groups. In PIT group, the 30 day mortality
was 23.7% vs. 8.6% for the MIT group. The 6 month mortality was 24.7
for PIT group and 9.9% for the MIT group (p value < 0.001). We then
used the Cox proportional hazards models to test the independent
effect of ischemic time on mortality while controlling for pre, peri
and post operative variables that were significantly associated with
ischemic time. Both the groups (MIT and PIT) were adjusted for
heart failure, prior PCI, preoperative dialysis, preexisting liver disease
and donor age in four quartiles. After adjusting the donor ischemic
time for these variables, the survival outcomes were not statistically
significant (The hazard ratio was 1.19 with 95% upper and lower CI
of 0.76 and 1.85, p value- 0.45, model 2). When both groups were
further adjusted for postoperative neurological outcomes, the hazard
ratio decreased further 1.13, p value-0.60 (model 3).
In this study, higher proportions of patients in PIT group have
had coronary intraluminal stenting procedures in the past (28.7
vs. 18.8, p value- 0.04). This could be because this group had more
advanced cardiac disease and ischemic burden. The PIT group also
had significantly more number of patients on dialysis (16.1 vs. 5.1,
p value < 0.001) and pretransplant liver dysfunction (11.8 vs. 2.5,
p value < 0.001) suggesting that they were in advanced stages of
cardiomyopathy with multiorgan dysfunction, thereby implying
more sicker patients comprising this group .We also had older
donors in the PIT group. This was statistically significant (12.2% in
PIT vs. 27.5% donors in MIT <21 years and 37.8 PIT vs. 23.8% MIT
donors >47 years, p value- 0.003). This is probably because even the
older donors were accepted for sicker recipients, considering the
urgently required donor organ in the PIT group. The duration of
cardiopulmonary bypass was longer in patients receiving a graft with
long ischemic time (mean of 355.4 minutes for PIT vs. 194.8 minutes
for MIT group, p< 0.001). This was because of planned longer
reperfusion time in patients with prolonged ischemic times. Although
univariate analysis did show significant mortality differences, when
we controlled both the groups for these above discussed variables
(prior PCI, pretransplant dialysis, pretransplant liver dysfunction,
donor age and duration of cardiopulmonary bypass), there were no
significant differences in survival outcomes between the two groups
[(hazardratiowas1.19 (model2)]. The decision to accept the donor
hearts from far off places with anticipated long ischemic times should
be a thoughtful process based on detailed evaluation of recipient
and donor specific factors. Variables such as recipient comorbidities
specially renal dysfunction and hepatic dysfunction, donor age, donor
inotropic use and left ventricular function should be considered in
the decision making process. Prolonged donor ischemic time in itself
should not be the deciding factor in not accepting the donor heart,
as the postoperative and survival outcomes are not much different
in patients with prolonged ischemic times. Our series also indicate
that donor hearts with prolonged ischemic times should not be
implanted to patients with advanced UNOS status and sicker hearts
along with other organ system dysfunction, as indicated by some
of the other studies [10-12]. In our series, the difference in survival
outcomes in univariate analysis was evident because of more sick
patients with multiorgan dysfunction in the PIT group but as both the
groups were controlled for other variables associated with prolonged
ischemic times, the survival outcomes were no different between
the groups. The largest single-center series to evaluate the effect of
prolonged donor ischemic times on transplant outcomes (in adult
population) evaluated donor ischemic time up to approximately 5
hours (295.5±37.1 minutes). Prolonged DIT was evaluated for up to
5 h in a cohort of 17 patients [22]. This study did not analyze whether
or not DIT >6 h adversely affected survival. The evidence evaluating
the impact of prolonged ischemia time in particular beyond 360 min,
on the short and long term outcomes after heart transplantation, is
limited and to our knowledge, has not been tested in adult cardiac
transplantation. In our study, we have shown that even extending
DIT beyond 6 h did not result in statistically significant differences in
survival outcomes. Although univariate analysis did show mortality
differences, there were no differences in survival outcomes between
the two groups after controlling for other pre, intra and post operative
variables that were significantly associated with ischemic time. This
study signals that in view of the current donor shortage, donor hearts
associated with anticipated prolonged ischemic times should be
considered as an option to expand the donor pool.
Conclusion
In summary, we can conclude that with the current techniques of myocardial preservation, modified reperfusion and the detailed evaluation of recipient and donor factors on a case by case basis, donor hearts with ischemia time greater than 6 h provide comparable postoperative outcomes and short, intermediate and long term survival results. The prolonged ischemic times, in itself, should not be a contraindication for OHT. Rather a thoughtful donor and recipient matching should be done and consideration should be given to the recipient UNOS status and comorbidities specially renal and hepatic dysfunction, donor age, donor cardiac function and stability.
References
- Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-44.
- Hertz MI. The Registry of the International Society for Heart and Lung Transplantation--Introduction to the 2012 annual reports: new leadership, same vision. J Heart Lung Transplant. 2012;31(10):1045-51.
- Keck BM, Bennett LE, Fiol BS, Daily OP, Novick RJ, Hosenpud JD. Worldwide thoracic organ transplantation: a report from the UNOS/ISHLT International Registry for Thoracic Organ Transplantation. Clin Transpl. 1998.
- Russo MJ, Chen JM, Sorabella RA, Martens TP, Garrido M, Davies RR, et al. The effect of ischemic time on survival after heart transplantation varies by donor age: an analysis of the United Network for Organ Sharing database. J Thorac Cardiovasc Surg. 2007;133(2):554-902.
- Taylor DO, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult heart transplant report – 2008. J Heart Lung Transplant 2008;27:943-56.
- Sievers HH, Leyh R, Jahnke A, Petry A, Kraatz EG, Herrmann G, et al. Bicaval versus atrial anastomoses in cardiac transplantation. Right atrial dimension and tricuspid valve function at rest and during exercise up to thirty-six months after transplantation. J Thorac Cardiovasc Surg. 1994;108(4):780-4.
- Leman NR, Levi DS, Alejos JC, Wetzel GT. Predictors of graft longevity in pediatric heart transplantation. Pediatr Cardiol. 2005;26:762–7.
- Mitropoulos FA, Odim J, Marelli D, Karandikar K, Gjertson D, Ardehali A, et al. Outcome of hearts with cold ischemic time greater than 300 minutes. A case-matched study. Eur J Cardiothorac Surg. 2005;28(1):143-8.
- Morgan JA, John R, Weinberg AD, Kherani AR, Coletti NJ, Vigilance DW, et al. Prolonged donor ischemic time does not adversely affect long-term survival in adult patients undergoing cardiac transplantation.J Thorac Cardiovasc Surg. 2003;126:1624–33.
- Young JB, Naftel DC, Bourge RC, Kirklin JK, Clemson BS, Porter CB, et al. Matching the heart donor and heart transplant recipient. Clues for successful expansion of the donor pool: a multivariable, multiinstitutional report. The Cardiac Transplant Research Database Group. J Heart Lung Transplant. 1994;13:353–65
- Bourge RC, Naftel DC, Costanzo-Nordin MR, Kirklin JK, Young JB, Kubo SH, et al. Pretransplantation risk factors for death after heart transplantation: a multiinstitutional study. The Transplant Cardiologists Research Database Group. J Heart Lung Transplant. 1993;12:549–62.
- Boehmer JP. Expanding the donor pool: how far is too far? J Heart Lung Transplant. 1993;12(5):816-8.
- Taylor DO, Edwards LB, Boucek MM, Trulock EP, Keck BM, Hertz MI. The Registry of the International Society for Heart and Lung Transplantation: Twenty-First Official Adult Heart Transplant Report—2004. J Heart Lung Transplant. 2004;23:796–803.
- Mullen JC, Bentley MJ, Modry DL, Koshal A. Extended donor ischemic times and recipient outcome after orthotopic cardiac transplantation. Can J Cardiol. 2001;17(4):421–6.
- Wahlers T, Cremer J, Fieguth HG, Dammenhayn L, Albes J, Schäfers HJ, et al. Donor heart-related variables and early mortality after heart transplantation. J Heart Lung Transplant. 1991;10(1 Pt 1):22-7.
- Del Rizzo DF, Menkis AH, Pflugfelder PW, Novick RJ, McKenzie FN, Boyd WD, et al. The role of donor age and ischemic time on survival following orthotopic heart transplantation. J Heart Lung Transplant. 1999;18(4):310-9.
- Young JB, Naftel DC, Bourge RC, Kirklin JK, Clemson BS, Porter CB, et al. Matching the heart donor and heart transplant recipient. Clues for successful expansion of the donor pool:a multivariable, multiinstitutional report. The transplant cardiologists research Database Group. J Heart Lung Transplant. 1994;13:353–65.
- Bourge RC, Naftel DC, Costanzo-Nordin MR, Kirklin JK, Young JB, Kubo SH, et al. Pretransplantation risk factors for death after heart transplantation: a multi-institutional study. The transplant cardiologists research Database Group. J Heart Lung Transplant 1993;12:549–62.
- Fernandez J, Aranda J, Mabbot S, Weston M, Cintron G. Overseas procurement of donor hearts: ischemic time effect on postoperative outcomes. Transplant Proc 2001;33:3803–4.
- Briganti EM, Bergin PJ, Rosenfeldt FL, Esmore DS, Rabinov M. Successful long-term outcome with prolonged ischemic time cardiac allografts. J Heart Lung Transplant. 1995;14(5):840-5.
- Adair JC, Call GK, O'Connell JB, Baringer JR. Cerebrovascular syndromes following cardiac transplantation. Neurology. 1992;42:819-23.
- Morgan JA, John R, Weinberg AD, Kherani AR, Colletti NJ, Vigilance DW, et al. Prolonged donor ischemic time does not adversely affect long-term survival in adult patients undergoing cardiac transplantation. J Thorac Cardiovasc Surg. 2003;126(5):1624-33.