Case Report
Tension Pneumothorax in Contralateral Lung during Left Video Assisted Thoracoscopic Surgery (VATS) Upper Lobectomy
Karim Morcos*, Sanjeet Singh, William Reeve and Mohammed Asif
Golden Jubilee National Hospital, National Waiting Times Centre, UK
*Corresponding author: Karim Morcos, Department of Cardiothoracic Surgery, Golden Jubilee National Hospital, Glasgow, UK
Published: 29 Dec, 2016
Cite this article as: Morcos K, Singh S, Reeve W, Asif M.
Tension Pneumothorax in Contralateral
Lung during Left Video Assisted
Thoracoscopic Surgery (VATS) Upper
Lobectomy. Clin Surg. 2016; 1: 1274.
Abstract
A Contralateral pneumothorax during surgery is a life=threatening emergency. We experienced a case of intraoperative right tension pneumothorax during a left sided lobectomy in a patient with multiple bullae, the discerning symptoms noted intraoperatively and the management of such an emergency.
Introduction
A 66 year old gentleman was referred to our unit following increasing shortness of breath on the background of previous asbestos exposure, COPD and 50-pack-year smoking history. Interval CT imaging revealed an enlarging speculated lesion in the left upper lobe. A PET scan confirmed a hypermetabolic 19 mm subpleural lesion with no evidence of metastasis.
Procedure
A standard 3-port VATS procedure was performed with the utility port placed anteriorly. The
lesion was excised as a wedge for a frozen section. It confirmed a non-small cell lung carcinoma
and an upper lobectomy performed. The left superior pulmonary vein, truncus anterior and
lingular branch of pulmonary artery were sequentially stapled and divided. The oblique fissure was
completed using diathermy. The upper lobe bronchus was then divided and stapled.
During reinflation to check for satisfactory left lower lobe ventilation, the patient started
desaturating and became hypotensive. Vasoconstrictors were bloused with little response. No endtidal-
CO2 was noted from the right lung on one lung ventilation. 3M™ Ioban™ incise drapes were
used to cover the left thoracotomy and the patient was placed supine.
A needle thoracostomy was performed and a hiss of air confirmed decompression of the tension
pneumothorax. His blood pressure and oxygen saturations improved thereafter. Diagnosis was
confirmed with CXR and a 28F chest drain was inserted into the right pleural cavity. The VATS
procedure was completed with the two further branches of the pulmonary artery to the upper lobe
stapled and divided. The lobe was retrieved via endobag. Washout was performed and haemostasis
confirmed. A 28F chest drain was placed via the camera port. Two paravertebral catheters were
inserted for post-operative analgesia. The remaining ports were closed with Vicryl sutures,
subcuticular Monocryl and Liquiband dressing.
Conclusion
Patients with bullous disease are at a higher risk of developing pneumothorax during surgery.
Clinical suspicion should dictate prompt immediate management to prevent adverse outcomes.
A pneumothorax is an abnormal collection of air within the pleural space resulting in
uncoupling of the lung from the chest wall [1]. This may or may not be accompanied by pain but
invariably presents as dyspnoea. They may occur spontaneously after a rupture of congenital bullae
or secondary to infection, trauma, malignancy or chronic obstructive pulmonary disease (COPD)
[2]. Tension pneumothorax occurs when there is a rapidly expanding collection of air in the pleural
space as a result of a one-way valve formed by the area of damaged tissue. Unless this is reversed
effectually in time, death may ensue [3]. Most trauma courses illustrate a patient in extremis thereby
giving the impression of straight-forward diagnosis that is reversed on needle thoracostomy but
this may not be the case in real life [4]. The literature describes many case reports whereby the‘classic’ signs of tension pneumothorax were absent thereby resulting
in missed initial diagnosis. In a trauma centre in London, tension
pneumothorax was confirmed in 5.4% of trauma patients by a hiss
of air on needle decompression. Of note, 64% of the patients were
ventilated [5]. We present a similar case in a patient undergoing a
left sided video assisted thoracoscopic lung resection who developed
a contralateral tension pneumothorax while undergoing single lung
ventilation.
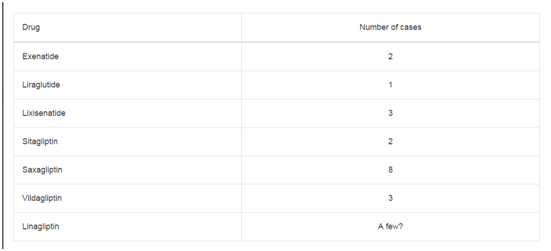
Table 1
Figure 1
Figure 2
Case Presentation
Tension pneumothorax intraoperatively is a rare phenomenon.
The Australian Incident Management System (AIMS) recorded that
of the 4000 reports sent, 65 mentioned pneumothorax as a potential
or actual diagnosis, and in 24, a pneumothorax was confirmed with
CXR [6]. The same group developed an algorithm for dealing with
such events called COVER ABCD-A SWIFT CHECK which is
described below (Table 1).
A 66 year old gentleman was referred to our Cardiothoracic
Unit following complaints of increasing shortness of breath on the
background of previous asbestos exposure. Other relevant history
includes being an ex-smoker with a 50 pack year history and
hypothyroidism. He had no noticeable weight loss or haemoptysis.
A chest radiograph (CXR) revealed irregular speculated opacity in
the left mid zone overlying the anterior aspect of the third rib. A
subsequent CT scan of the thorax, abdomen and pelvis revealed the
speculated 11mm lesion to be a possible post inflammatory scarring/
rounded atelectasis or early bronchial carcinoma on the background
of bilateral bullous disease.
A repeat scan done 3 months later revealed an enlarging lesion
that measured 12 x 12 x 12 mm with the presence of an enlarged hilar
node that was not previously noted. A full body PET scan revealed
a hypermetabolic 19 mm subpleural speculate lesion within the left
lung's upper lobe in keeping with malignancy with no evidence of
metastasis and was suitable for resection. His MRC dyspnea grade was
2 and performance status was 1. He was able to walk approximately
300-400 yards before becoming short of breath and mobilised up and
down 2 flights of stairs daily with no limitations. His FEV1 was 86%
of the predicted. He was listed for a VATS lobectomy.
Procedure
His preoperative period was uneventful. General anesthesia was
induced. The patient was intubated with a left-sided 35F doublelumen
tube (DLT) without difficulty and was placed in a right
lateral decubitus position. A standard 3 port VATS procedure was
performed with the utility port placed anteriorly. The lesion was
noted on insertion of the thoracoscope and excised as a wedge using
a tri-stapler and sent for a frozen section. The preliminary report was
in keeping with non-small cell lung carcinoma and thus a left upper
lobectomy was carried out.
The left superior pulmonary vein was dissected and then stapled
and divided. The truncus anterior and lingular branch of the
pulmonary artery were stapled and divided followed by completion of
the oblique fissure anteriorly using electrocautery. The left upper lobe
bronchus was finally divided using the stapler. During reinflation of
the lung to check for satisfactory Left Lower Lobe ventilation, the
patient started desaturating despite an expanding lower lobe. He
was noted to be hypotensive as well. A bolus of vasoconstrictors was
administered by the anaesthetist with little response. No end tidal
CO2 was noted in the right lung on one lung ventilation.
The position of the endotracheal tube was confirmed by flexible
bronchoscopy and was satisfactory.
A clinical diagnosis of potential right tension pneumothorax
was made. 3M™ Ioban™ incise drapes were used to cover the left
thoracotomy and the patient was placed on his back.
A 14 G Cannula was inserted in the 3rd intercostal space in the
mid-clavicular line and a hiss of air confirmed decompression of the
tension pneumothorax. His blood pressure and Oxygen saturations
improved thereafter. The diagnosis was confirmed with a CXR and
a 28 F chest drain was inserted into the right pleural cavity. The
patient was then repositioned on his side and the VATS procedure
was continued. The two further branches of the pulmonary artery
to the upper lobe; each one was stapled and divided using tristapler
and vascular staples. The remaining very small part of the
oblique fissure posteriorly was completed with blunt dissection.
The lobe was then removed using an Endocatch bag. Washout was
performed and haemostasis checked and secured. A single 28 French
chest drain was left in situ via the camera port. Two paravertebral
catheters were inserted for post-operative analgesia. The utility port
and the remaining port were closed with Vicryl sutures, subcuticular
Monocryl and Liquiband tissue dressing.
Postoperatively, he was required re-intubation and a suction
bronchoscopy due to difficulty re-inflating the right lung. Once
extubated, he had some epigastric tenderness post operatively treated
with IV proton pump inhibitors (PPIs) as per the Hong Kong regime.
He was then commenced on oral PPIs once his symptoms settled
within 2 days. He was subsequently discharged on post-operative day
7. At follow up in 6 weeks, his wounds had healed well and his CXR
revealed some pleural thickening in the left base and reduced lung
volume on the operated side but nil else of note.
Figure 3
Figure 4
Discussion
Diagnosis of tension pneumothorax especially in ventilated
patients can be challenging. Progression of a simple pneumothorax
to a tension pneumothorax is more likely in a ventilated patient and
is associated with a higher mortality, quoted at 91% in one series [7].
In a patient with an open thorax, the classic signs of decreased
O2 saturation and increasing difficulty in ventilation and circulatory
collapse may be blunted due to the lack of a mediastinal shift and
compression; thereby not causing distortion of the great vessels as the
one-way valve effect is mitigated by the thoracotomy 2.
Despite this, contralateral tension pneumothorax during
thoracotomy is a rare phenomenon. However due to the fragility of
emphysematous bullae in our patient, even a small amount of positive
pressure ventilation could cause a rupture secondary to barotrauma.
Other potential causes include pleural punctures from central line
insertion, epidural needle insertion and damage to the bronchus
during introduction of the bronchial tube [8].
A review conducted by Leigh-Smith et al. (2000) looked at the
causes of tension pneumothorax in ventilated patients from casereports.
Universal findings in most case reports describing tension
pneumothorax in ventilated patients include rapid onset, immediate
and progressive decrement in arterial and mixed venous SpO2,
and immediate reduction in cardiac output with or without blood
pressure changes. A high index of suspicion is also needed especially
in patients with emphysematous disease bilaterally.
References