Case Report
Postoperative Infection Caused by a Resorbable Plate used to Treat a Zygomatic Fracture
Sukegawa S1*, Kanno T1,2, Kawai H3, Shibata A1, Sukegawa-Takahashi Y1 and Furuki Y1
1Division of Oral and Maxillofacial Surgery, Kagawa Prefectural Central Hospital,Japan
2Department of Oral and Maxillofacial Surgery, Shimane University Faculty of Medicine, Japan
3Department of Oral Pathology and Medicine, Okayama University, Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Japan
*Corresponding author: Shintaro Sukegawa, Division of Oral and Maxillofacial Surgery, Kagawa Prefectural Central Hospital, 1-2-1, Asahi-cho, Takamatsu, Kagawa 760-8557, Japan
Published: 12 May, 2016
Cite this article as: Sukegawa S, Kanno T, Kawai H,
Shibata A, Sukegawa-Takahashi Y, Furuki Y. Postoperative Infection Caused by a Resorbable Plate used to Treat a Zygomatic Fracture. Clin Surg. 2016; 1: 1002.
Abstract
A 58-year-old female patient was referred to our division of Oral and Maxillofacial Surgeryby a
general dental practitioner with swelling symptoms in the left cheek. Five months earlier, she had
fractured her left zygomatic bone, which was fixed using a resorbable plate. A maxillofacial computed
tomographic scan taken upon the first visit showed a clear swelling of the soft tissue next to the left
maxillary sinus and a maxillary sinusitis. In addition, the plate at the zygomaticomaxillary buttress
showed bone resorption surrounding the plate and the screws, possibly because of an infection
affecting the area around both the plate and the screws. These were removed, and their molecular
weight and average molecular weight measured following extraction. These measurements showed
that the plate and the screws had progressively degraded. All symptoms immediately diminished
after the operation and no evidence of infection was observed after 3 months after the operation.
Keywords: Resorbable plate; Postoperative infection; Molecular weight
Introduction
Maxillofacial fractures are commonly fixed using titanium mini plates because they are strong,
easy to handle, and are not prone to dimensional changes [1,2]. However, fracture fixation using
titanium plates present some disadvantages, including potential difficulties associated with the
subsequent removal surgery, facial growth [3,4], thermal sensitivity [5,6], and plate migration [7,8],
ultimately leading to the development of resorbable bone fixation devices as a trend.
Bioresorbable plates are designed to be absorbed by the surrounding tissue through chemical
interactions; therefore, negative foreign body reactions and infection throughout the resorption
process are theoretically possible [5]. However, there are little complications involved and it is used
by clinicians as a major device [9,10].
This report presents a case of infection, following zygomatic fracture fixation using a resorbable
plate, suspected of being caused by the resorption process.
Presentation of Case
In June 2014, a 58-year-old female patient who did not present any note worthy past medical
condition was referred to our division of Oral and Maxillofacial Surgery, Kagawa Prefectural
Central Hospital, Takamatsu, Kagawa, Japan by a general dental practitioner because of swelling
in the left cheek. Five months earlier, the patient underwent surgery
to fit a Lactosorb® 1.5 resorbable fixation system (Lorenz Surgical,
Jacksonville, FL, USA) to fix a zygomatic bone fracture at another
general hospital. The patient never suffered any discomfort or
presented any problems in the operative site before the fracture.
Osteosynthesis was achieved by a fixation technique using three
points along to the orbital rim, the frontozygomatic suture, and the
zygomaticomaxillary buttress. During her first visit to the general
dental practitioner, an intraoral examination revealed the presence of
pus, discharged from the gingivobuccal area (Figure 1). Furthermore,
a probe showed that the bone could be easily reached. A maxillofacial
computed tomographic scan taken during the first visit showed as
welling of the soft tissue next to the left maxillary sinus and a maxillary
sinusitis. In addition, the plate at the zygomaticomaxillary buttress
showed bone resorption surrounding the plate and the screws (Figure 2).
These clinical symptoms did not improve after initial treatment
with Clarithromycin for 2 weeks, followed by Cefcapenepivoxil
hydrochloride hydrate for 2 weeks together with continuous local
irrigation. Based on these symptoms the patient was diagnosed with
an infection caused by the fitted resorbable plate and screw, and the
full removal of biomaterials was recommended. The patient was
operated to remove the plate and the screws under local anesthesia.
The operation involved a vestibular incision on the left side of the
mandible to locate and remove the free resorbed plate and the screws
on the buttress. In addition, the operative team cleaned the area of
bone resorption surrounding the bioresorbable plate and the maxillary
sinus front wall for abscess formation of the maxillary sinus (Figure
3). During the operation, we took samples from the affected area;
Streptococcus milits and anaerobic bacteria were cultured from these
samples. The patient reported an immediate relief of the symptoms
after the operation, and no evidence of infection was detected after
3months of follow-up.
Figure 1
Figure 1
(A) Frontal aspect at admission, showing the intact facial skeleton
with enophthalmos of the left eye. (B) Coronal and (C) Sagittal computed
tomography images showing a defect in the mid-left orbital floor, with
herniation of the orbital contents into the underlying maxillary sinus.
Figure 2
Figure 2
A titanium mesh plate with high three-dimensional flexibility was
designed to create a basic hexagonal polygon shape.
Figure 3
Figure 3
The implant was designed using a rapid prototype threedimensional
model that mirrored the shape of the intact opposite orbit. It was
designed to precisely cover the bony defect and support the orbital globe.
Figure 4
Figure 4
The preshaped titanium mesh plate was positioned to support the
orbital globe in the left orbital floor. Because the implant conformed perfectly
to the shape of the intact bone around the defect, positioning of the plate
was easy.
Measurement of the Molecular Weight
To measure the molecular weight (Mw) of the extracted plate
and screws, they were dissolved in tetrahydrofuran. Gel permeation
chromatography using a TOSOH Build-up GPC system 8020 and a
TOSOH Co, Japan) and a TSK-GELGMHHR-H (TOSOH Co, Japan)
was used to estimate the molecular weight. This technique is able to
separate polymers based on their size. Polystyrene (SM-105 by Showa
Denko Co, Japan) was used for Mw calibration. For comparative
purposes, the molecular weight of an intact Lactosorb®
plate and
screws were also measured following the same protocol.
The average molecular weight (Mn) was calculated using the
following equation:
Mn=Σ (Mi·Ni)/ΣNi
Where Mi represents the molecular weight and Ni the number of
numerators of the polymer.
The weighted average molecular weight (Mw) was calculated
using the following equation.
Mw=Σ (Mi2·Ni)/Σ(Mi·Ni)
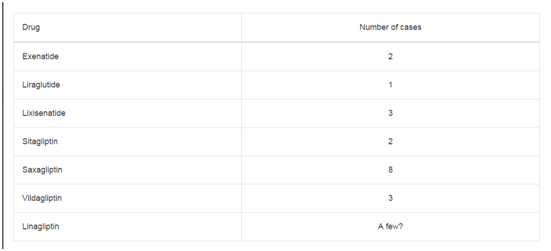
The plate removed 5 months after the initial surgery showed an
average molecular weight and a weighted average molecular weight of
2.28 × 104
and 5.36 × 104
, respectively. This represents a 53% decrease
in Mn and a 54% decrease in Mw compared with an intact plate. Mn
and Mw of the two screws removed were 2.01 × 104
, and 2.19 × 104, and 5.27 × 104
, and 5.59 × 104
, respectively. These values indicated
that Mn decreased by 58% and 54% for the first and second screw,
respectively, and Mw had decreased by 56% and 54% compared with
intact screws (Table 1).
Table 1
Discussion
Resorbable Osteosynthes is systems were well developed to
replace titanium fixation systems in craniofacial, oral, maxillofacial,
plastic, and reconstructive surgery [1,2]. The resorbable materials
used are ideally able to meet the biomechanical demands and to
provide enough initial strength; however, these materials are able
to degrade in a predictable manner throughout the healing process,
providing sufficient strength and biomechanical stability to ensure
the full healing of the fractured section. This resorption process has
the added advantage of eliminating the need to remove the plate or
the screws because no deleterious bodily response is associated with
the presence of these materials or the resorption process [11].
The resorbable materials are designed to undergo a biphasic
degradation process, including an early degradation step via hydrolysis
of ester bonds [9,12]. The resulting degradation products subsequently
crystallize and undergo a secondary hydrolysis, which strongly
determines the rate of degradation of the material [12]. Throughout
this process, the molecular weight of the material progressively
decreases to eventually disappear. This degradation process is
associated with a decrease in polymer strength [11], a reduction in
molecular weight, and strength and mass loss. The implants lose the
clinical biomechanical properties long before the loss of a significant
amount of mass. The final end products of this degradation process,
CO2 and H2O, are ultimately metabolized by the liver [9]. In this case,
a LactoSorb (Lorenz/Biomet Inc.) bioresorbable system was used,
which was composed by a substantially amorphous linear copolymer
and consisted of 82% PLLA and 18% PGA. This material is able to
retain 70% of its initial strength for the first 6–8 weeks, and it has
been reported to dissolve entirely within the first year [13]. In this
case, the patient had healed well after 5 months, and the bioresorbable
system appeared to be efficient as Osteosynthesis material. However,
bone resorption was observed around the bioresorbable plate and the
screws fitted to the zygomatic and the maxillary bones. Inflammation
could be expected for those cases where the degradation rate is too
high and debris particles are produced faster than the body can
tolerate [14]. The strong inflammatory reaction in the implantation
site observed in this case was possibly caused by an increase in
degradation products. This degradation probably caused the
disintegration of the implanted materials, leading to the infiltration of
the polymer into the adjacent tissues, overwhelming local clearance
mechanisms. The molecular weight of the removed plate was 53%
lower (58 and 52% lower for the screws) compared with intact plates,
indicating that the absorption of the Osteosynthesis material had
progressed as expected. The severe inflammation reaction observed
could have led to periimplant osteolysis. In addition, the mobility
of the plate and the screw as a result of the bone resorption could
have further exacerbated the maxillary infection. A buccal buttress
requires an occlusal stress. Resorption of a plate progresses 5 months
postoperatively and the plate strength decreases. Because an occlusal
force is recovered 2 months postoperatively for zygomatic fractures
[15], it may lead to instability of a plate by a strong occlusal stress.
Therefore, during zygomatic fracture treatment, we have to consider
buccal buttress of the resorptive plate in which strength temporally
reduces. To prevent the plate surge by an incongruity, it is required to
firmly fit a plate to a bone.
This plate system has been widely and successfully used as an
Osteosynthesis material [9]. In this case, the same plate system was
used for other sites, such as the orbital rim and the zygomaticofrontal
suture; however, bone resorption was only observed in the
zygomaticomaxillary suture, connected to the side of the oral cavity.
The presence of an oral Streptococcus sp. infection suggests an oral
origin of the infection. This bacterial infection may have promoted
the resorption of the bone surrounding the plate system, worsening
the situation. Although inflammation by a foreign-body reaction
occurs, there is generally little bacterial infection at areas other than
the oral cavity. Because the oral-cavity is always exposed to the oral
origin bacteria, we should be cautious regarding infections occurring
at a relatively early stage.
Conclusions
Here postoperative complications related to the biodegradation of resorbable materials are reported. This study shows that there is a need to widen our understanding on the characteristics and use of these resorbable materials based on clinical observations.
References
- Bos RR. Treatment of pediatric facial fractures: The case for metallic fixation. J Oral Maxillofac Surg. 2005; 63: 382-384.
- Eppley BL, Sadove AM. Effects of resorbable fixation on craniofacial skeletal growth: Modifications in plate size. J Craniofac Surg. 1994; 5: 110-114.
- Eppley BL, Platis JM, Sadove AM. Experimental effects of bone plating in infancy on cranio maxillofacial skeletal growth. Cleft Palate Craniofac J. 1993; 30: 164-169.
- Yaremchuk MJ, Fiala TGS, Barker F, Ragland R. The effects of rigid fixation on craniofacial growth of rhesus monkeys. Plast Reconstr Surg. 1994; 93: 1-10.
- Eppley BL, Sparks C, Herman E, Edwards M, McCarty M, Sadove AM. Effects of skeletal fixation on craniofacial imaging. J Craniofac Surg. 1993; 4: 67-73.
- Manson PN, Hoopes JE, Su CT. Structural pillars of the facial skeleton: An approach to the management of Le Fort fractures. Plast Reconstr Surg. 1980; 66: 54-62.
- Fearon JA, Munro IR, Bruce DA. Observations on the use of rigid fixation for craniofacial deformities in infants and young children. Plast Reconstr Surg. 1995; 95: 634-637.
- Yu JC, Bartlett SP, Goldberg DS, Gannon F, Hunter J, Habecker P, et al. An experimental study of the effects of craniofacial growth on the long-term positional stability of microfixation. J Craniofac Surg. 1996; 7: 64-68.
- Bell RB, Kindsfater CS. The use of biodegradable plates and screws to stabilize facial fractures. J Oral Maxillofac Surg. 2006; 64: 31-39.
- Sukegawa S , Kanno T, Katase N, Shibata A, Takahashi Y, Furuki Y. Clinical evaluation of an unsintered hydroxyapatite/poly-L-lactide osteoconductive composite device for the internal fixation of maxillofacial fractures. J Craniofac Surg. 2016 in press
- Pietrzak WS, Sarver DR, Verstynen ML. Biosorbable polymer science for the practicing surgeon. J Craniofac Surg. 1997; 8: 87-91.
- van der Elst M, Klein CP, de Blieck-Hogervorst JM, Patka P, Haarman HJ. Bone tissue response to biodegradable polymers used for intra medullary fracture fixation: a long-term in vivo study in sheep femora. Biomaterials. 1999; 20: 121-128.
- Eppley B, Sadove A. A comparison of resorbable and metallic fixation in healing of calvarial bone grafts. Plast Reconstr Surg. 1995; 96: 316-322.
- Wittwer G, Adeyemo WL, Yerit K, Voracek M, Turhani D, Watzinger F, et al. Complications after zygoma fracture fixation: is there a difference between biodegradable materials and how do they compare with titanium Osteosynthesis?. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101: 419-425.
- Ribeiro MC, Regalo SC, Pepato AO, Siéssere S, de Souza LG, Sverzut CE, et al. Bite force, electromyography, and mandible mobility during the 6-month period after surgical treatment for isolated fractures of the zygomatico-orbital complex. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111: 1-7.